Nurses protested at hospitals on March 23 over a shortage of masks and protective gear.David Crane/ZUMA
This story is from the Center for Public Integrity, a nonprofit, nonpartisan investigative media organization in Washington, D.C.
More than 3,000 nurses from across the country gathered the afternoon of March 12 for a critical conference call.
The nurses wanted answers from their union leaders: Could people build immunity to the coronavirus? How long does the virus stick to surfaces? What’s the best way to protect themselves from contracting COVID-19?
Although nearly two weeks had passed since the United States’ first coronavirus patient died outside of Seattle, many nurses on this call still found themselves awash in conflicting information about how to stay safe. Union leaders tried to set the record straight.
As of Sunday, more than 2,400 people across the nation have died from COVID-19, and more than 135,000 have tested positive for it. Nurses and other health care workers are at high risk of contracting the disease, and they’re panicking, saying hospitals and the government aren’t doing enough to limit their exposure.
Despite such concerns, the U.S. Department of Labor has refused to issue an emergency rule requiring hospitals to create a plan to protect their employees from exposure to the coronavirus and other infectious diseases, according to records obtained by the Center for Public Integrity.
And the federal agency’s Occupational Safety and Health Administration won’t provide direction to its safety inspectors on how to cite hospitals and nursing homes that aren’t doing enough to protect workers from the new hazard—a departure from its practice during past outbreaks.
Meanwhile, the hospital industry’s trade group, the American Hospital Association, has successfully lobbied Congress to block passage of an emergency infectious disease standard that would strengthen protections for health care workers on the front lines. Earlier this month, House lawmakers scrapped language from a relief bill that would have forced the Department of Labor to create one.
The result: Nurses and other health care workers say they’re left to fend for themselves.
“It’s frightening,” said Katie Oppenheim, a nurse in Michigan, noting that her hospital recently began giving nurses less protective masks than the N95 respirators they’ve been wearing. Others say their hospitals won’t test employees who’ve been exposed to the coronavirus.
A recent survey of 8,200 nurses, conducted by three nursing groups, showed that less than half had been briefed about COVID-19 by their supervisors.
The resistance to employee protections comes as more and more U.S. health care workers get sick.
It’s unclear how many medical personnel have been infected by the coronavirus—the Centers for Disease Control and Prevention did not respond to a request for the information from Public Integrity. But media reports have identified more than 100 cases, including those involving a nurse in Connecticut and two emergency physicians in New Jersey. At least one nurse, in New York City, has died from the disease. His co-workers blamed the hospital for not providing him with appropriate protective gear. Two health care workers have also died amid the shortage of protective gear in Georgia.
Hundreds of other health care workers have been quarantined from exposure to the coronavirus at work.
There are about 18 million health care workers in the United States. Women make up the vast majority.
“This is a desperate situation, and the lives of health care workers are at stake,” said David Michaels, who led OSHA until 2017 and now teaches environmental and occupational health at The George Washington University. They “have to be the first ones protected.”
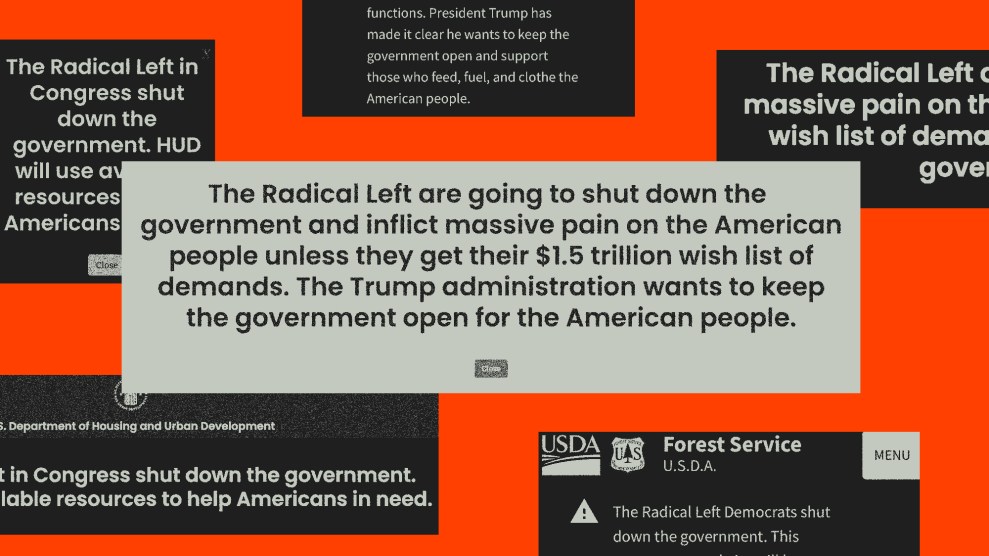
The Department of Labor’s refusal to issue an emergency rule aligns with the Trump administration’s overarching deregulation efforts. Workplace safety experts warn that the threat of fines and bad publicity from an OSHA citation is exactly what’s needed to make hospitals take care of their employees during the pandemic. The lack of enforcement action by OSHA, they say, is putting the lives of health care workers at risk, increasing the chances that they’ll spread the disease to their families and communities.
OSHA Refuses to Act
It’s possible that, a decade ago, Department of Labor officials foresaw the current crisis.
In 2010, OSHA started drafting a new safety standard that would require health care employers to create infection control plans to keep doctors, nurses and other health care workers from getting exposed to deadly diseases. That could mean building isolation rooms to quarantine patients and making sure employees wear gowns, gloves and respirators around high-risk patients.
The nation had just escaped the worst of the H1N1 swine flu, which killed more than 12,000 Americans and infected 48 health care workers. At the time, OSHA had a rule to protect health care workers from bloodborne infections — such as hepatitis — but nothing for respiratory infections, which is what COVID-19 is.
The safety standard wound its way through the rulemaking process. The Department of Labor issued a draft in early 2017. A few months later, after Donald Trump took office, the Department of Labor punted it to the agency’s “long-term” regulatory agenda. Nothing has happened since.
Fast forward three years. With COVID-19 paralyzing the country, labor unions and workers’ rights advocates have been urging OSHA to issue an emergency version of the rule right away.
On March 5, Reps. Bobby Scott, D-Va., and Alma Adams, D-N.C., sent a letter to Labor Secretary Eugene Scalia demanding the same action.
“If healthcare workers are quarantined in large numbers, or get ill or die, or fear coming to work due to the risks, it’s not just a workplace problem, it’s a national public health disaster,” they wrote.
But OSHA has since made clear that it won’t comply.
Loren Sweatt, who leads OSHA, responded in a March 18 letter that the emergency rule would “distract” hospitals from fighting the coronavirus.
“OSHA believes that the healthcare industry fully understands the gravity of the situation and is taking appropriate steps to protect its workers while responding to the public health emergency,” Sweatt responded in the letter, which Public Integrity obtained.
House lawmakers had also urged OSHA to issue what is known as a “compliance directive” to tell its safety inspectors how to issue citations against health care providers that don’t do enough to protect workers from the coronavirus. The agency issued similar directives to deal with tuberculosis outbreaks and, again, with the swine flu.
The swine flu directive, 46 pages in all, was issued in November 2009. For example, it specifically directed inspectors of hospitals and nursing homes to determine if facility managers briefed their employees about the new virus and whether they trained nurses how to deal with patients who are showing symptoms.
If hospitals and nursing homes failed the test, then OSHA could cite them and fine them.
In her letter, Sweatt noted that OSHA inspectors would continue enforcing the laws that are already on the books, like making sure hospitals record every work-related illness.
“OSHA can and will use enforcement, as necessary, to ensure the protection of workers exposed to COVID,” she wrote.
But the emergency rule could have made many of the safety guidelines from the CDC legally binding.
Hospitals and clinics receiving Medicaid and Medicare funding must have an infectious disease control plan, but the rule is rarely enforced, experts say. And research suggests that many hospitals don’t always do what they should to protect their employees from infections such as COVID-19.
A 2008 study by researchers at the University of Washington and the Washington State Department of Health, for example, found “significant gaps” in compliance with the CDC guidelines at five hospitals in the Seattle area, noting that their employees failed to use appropriate protective gear and were not properly trained.
California is the only state that has a binding standard to protect health care workers from infectious diseases. Still, nurses in the state have complained that hospitals aren’t taking all the steps they’re supposed to.
Cathy Kennedy, a registered nurse at Kaiser Permanente Roseville Medical Center in California, said staff members asked hospital managers in February to share their infection control plan and train them to stay safe. The hospital did not, she said.
Then, on March 4, the hospital reported the first coronavirus death in the state: An elderly man who had recently traveled on a Princess Cruises ship.
“You would also think that, after the first patient died, they would take our request seriously. They did not,” Kennedy, who is vice president of National Nurses United, said on the March 12 conference call with other nurses. “We are still trying to figure out what are the protocols at my facility.”
The confusion created by the coronavirus is one reason why nurses have been pushing for the emergency rule. But the hospital industry has successfully blocked efforts in Congress to force OSHA to issue one.
Congress Spikes Safety Provisions
A decade ago, the American Hospital Association lobbied successfully against OSHA’s proposed infectious disease rule. The hospital industry’s trade association is one of the most heavily financed lobbying groups in the nation, spending $26.2 million in 2019 alone.
Now, it has helped keep safety standards out of several coronavirus relief bills in Congress.
On March 12, the trade group sent out an email alert warning its members that the House’s Families First Coronavirus Response Act had an unpleasant surprise: a provision called the Health Care Worker Protection Act, which would force OSHA to create an emergency safety standard to shield workers from COVID-19.
That rule would have required hospitals and nursing homes to create a plan to protect their employees from infections and to provide nurses and doctors with respirators. It would have also allowed OSHA to apply the safety standard to others at high risk of contracting the virus, such as home health aides.
The provision had broad support from workplace safety advocates and labor unions, but the hospital industry wasn’t having it.
“This provision would be impossible to implement in hospitals due to the severe lack of availability of N95 respirators,” the American Hospital Association’s alert said. “If this provision were to be enacted, hospital inpatient capacity would be dramatically reduced.”
The trade group, which represents nearly 5,000 hospitals and other health care providers across the country, did not respond to a request for comment.
An aide on the House Committee on Education and Labor said the provision wouldn’t have punished hospitals and nursing homes for equipment shortages, as long as they made an effort to find protective gear. The aide, who spoke on the condition of anonymity to speak frankly about the issue, said the provision was taken out at the last minute from the bill.
The latest stimulus bill in the Senate doesn’t include the safety standard, but a recent proposal from House Speaker Nancy Pelosi, D-Calif., does.
As the tug of war over workplace protections continues, Europe has provided a glimpse of what could come. In Spain, about 14 percent of people infected with COVID-19 are health care workers, putting a strain on staffing at hospitals. In Italy, about 8 percent of medical professionals have tested positive for the disease.
Rebecca Reindel, director of health and safety for the AFL-CIO labor federation, said the government doesn’t seem to grasp the urgency of the moment.
“This is seriously problematic,” she said. “The administration didn’t have protections in place, was slow to act on any sort of guidance coming out, and then it took them a while to get going.”
Nurses are now lobbying for themselves.
Bonnie Castillo, executive director of National Nurses United, spoke in a somber tone on the March 12 call with thousands of nurses.
“I know that nurses and other health care workers are feeling a lot of frustration and concern right now,” Castillo said. “The response we’ve all seen right now to COVID-19 has obviously not been a success.”
She listed all the targets they’ve lobbied to pass worker protections: the CDC, the Department of Labor, the White House, every legislator in Congress.
“We are not going to stand back,” she said. “We’re not going to be silent and let our employers or our government agencies put us in harm’s way.”
So far, the pressure hasn’t worked.