Jacqueline Larma / AP
This story was originally published by ProPublica.
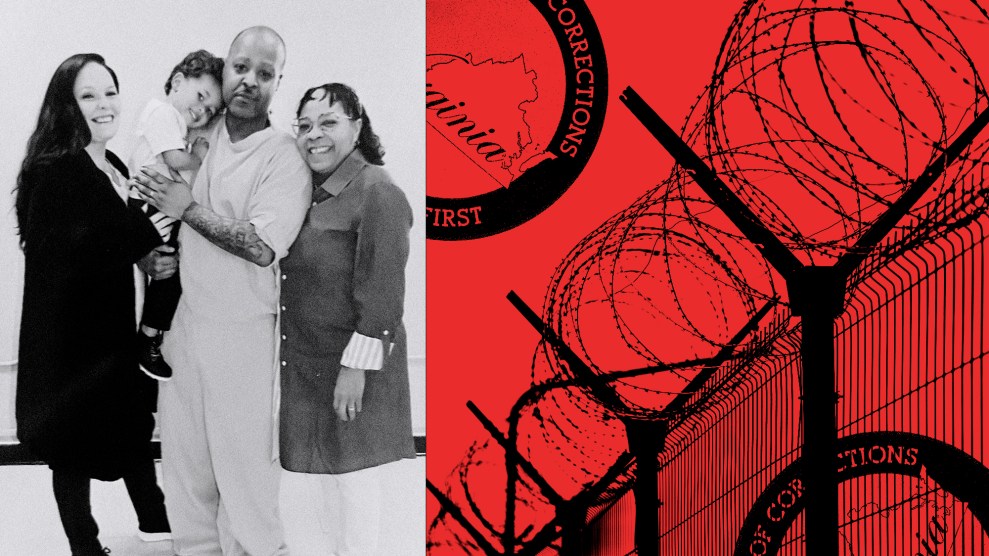
Ever since her 14-year marriage imploded in financial chaos and a protective order, Amy Lankford had kept a wary eye on her ex, David Williams.
Williams, then 51, with the beefy body of a former wrestler gone slightly to seed, was always working the angles, looking for shortcuts to success and mostly stumbling. During their marriage, Lankford had been forced to work overtime as a physical therapist when his personal training business couldn’t pay his share of the bills.
So, when Williams gave their three kids iPad Minis for Christmas in 2013, she was immediately suspicious. Where did he get that kind of money? Then one day on her son’s iPad, she noticed numbers next to the green iMessage icon indicating that new text messages were waiting. She clicked.
What she saw next made her heart pound. Somehow the iPad had become linked to her ex-husband’s personal Apple device and the messages were for him.
Most of the texts were from people setting up workouts through his personal training business, Get Fit With Dave, which he ran out of his home in Mansfield, Texas, a suburb of Fort Worth. But, oddly, they were also providing their birthdates and the group number of their health insurance plans. The people had health benefits administered by industry giants, including Aetna, Cigna and UnitedHealthcare. They were pleased to hear their health plans would now pay for their fitness workouts.
Lankford’s mind raced as she scrolled through the messages. It appeared her ex-husband was getting insurance companies to pay for his personal training services. But how could that be possible? Insurance companies pay for care that’s medically necessary, not sessions of dumbbell curls and lunges.
Insurance companies also only pay for care provided by licensed medical providers, like doctors or nurses. Williams called himself “Dr. Dave” because he had a Ph.D. in kinesiology. But he didn’t have a medical license. He wasn’t qualified to bill insurance companies. But, Lankford could see, he was doing it anyway.
As Lankford would learn, “Dr. Dave” had wrongfully obtained, with breathtaking ease, federal identification numbers that allowed him to fraudulently bill insurers as a physician for services to about 1,000 people. Then he battered the system with the bluntest of ploys: submit a deluge of out-of-network claims, confident that insurers would blindly approve a healthy percentage of them. Then, if the insurers did object, he gambled that they had scant appetite for a fight.
By the time the authorities stopped Williams, three years had passed since Lankford had discovered the text messages. In total, records show, he ran the scheme for more than four years, fraudulently billing several of the nation’s top insurance companies—United, Aetna and Cigna—for $25 million and reaping about $4 million in cash.
In response to inquiries, Williams sent a brief handwritten letter. He didn’t deny billing the insurers and defended his work, calling it an “unprecedented and beneficial opportunity to help many people.”
“My objective was to create a system of preventative medicine,” he wrote. Because of his work, “hundreds of patients” got off their prescription medication and avoided surgery.
There are a host of reasons health care costs are out-of-control and routinely top American’s list of financial worries, from unnecessary treatment and high prices to waste and fraud. Most people assume their insurance companies are tightly controlling their health care dollars. Insurers themselves boast of this on their websites.
In 2017, private insurance spending hit $1.2 trillion, according to the federal government, yet no one tracks how much is lost to fraud. Some investigators and health care experts estimate that fraud eats up 10% of all health care spending, and they know schemes abound.
Williams’ case highlights an unsettling reality about the nation’s health insurance system: It is surprisingly easy for fraudsters to gain entry, and it is shockingly difficult to convince insurance companies to stop them.
Williams’ spree also lays bare the financial incentives that drive the system: Rising health care costs boost insurers’ profits. Policing criminals eats away at them. Ultimately, losses are passed on to their clients through higher premiums and out-of-pocket fees or reduced coverage.
Insurance companies “are more focused on their bottom line than ferreting out bad actors,” said Michael Elliott, former lead attorney for the Medicare Fraud Strike Force in North Texas.
As Lankford looked at the iPad that day, she knew something else that made Williams’ romp through the health care system all the more surprising. The personal trainer had already done jail time for a similar crime, and Lankford’s father had uncovered the scheme.
Scanning her ex-husband’s texts, Lankford, then 47, knew just who to call. During the rocky end of her marriage, her dad had become the family watchdog. Jim Pratte has an MBA in finance and retired after a career selling computer hardware, but even the mention of Williams flushed his face red and ratcheted up his Texas twang. His former-son-in law is the reason he underwent firearms training.
Lankford lived a few minutes away from her parents in Mansfield. She brought her dad the iPad and they pored over message after message in which Williams assured clients that their insurance would cover their workouts at no cost to them.
Lankford and Pratte, then 68, were stunned at Williams’ audacity. They were sure the companies would quickly crackdown on what appeared to be a fraudulent scheme.
Especially because Williams had a criminal record.
In early 2006, while Williams and Lankford were going through their divorce, the family computer started freezing up. Lankford asked her dad to help her recover a document. Scrolling through the hard drive, Pratte came upon a folder named “Invoices,” and he suspected it had something to do with Williams.
His soon to be ex-son-in-law had had a promising start. He’d wrestled and earned bachelor’s and master’s degrees at Boise State University, and a Ph.D. at Texas A&M University, before landing a well-paying job as a community college professor in Arlington. But the glow faded when the school suddenly fired him for reasons hidden by a confidential settlement and by Williams himself, who refused to reveal them even to his wife.
Out of a job, Williams had hustled investments from their friends to convert an old Winn-Dixie grocery store into a health club called “Doc’s Gym.” The deal fell apart and everyone lost their money. The failure was written up in the local newspaper under the headline: “What’s up with Doc’s?”
Inside the “Invoices” folder, Pratte found about a dozen bills that appeared to be from a Fort Worth nonprofit organization where his daughter and Williams took their son Jake for autism treatment. As Pratte suspected, the invoices turned out to be fake. Williams had pretended to take Jake for therapy, then created the false bills so he could pocket a cash “reimbursement” from a county agency.
In November 2008, Williams pleaded guilty in Tarrant County District Court to felony theft. He was sentenced to 18 months in jail and was released on bail while he appealed.
Things took an even darker turn about two years later when Williams and Lankford’s 11-year-old son showed up to school with bruising on his face. Investigators determined that Williams had hit the boy in the face about 20 times. Williams pleaded guilty to causing bodily injury to a child, a felony, which, coupled with the bail violation, landed him in jail for about two years.
The time behind bars didn’t go to waste. Williams revised the business plan for Get Fit With Dave, concluding he needed to get access to health insurance.
Williams detailed his plans in letters to Steve Cosio, a tech-savvy friend who ran the Get Fit With Dave website in exchange for personal training sessions. Cosio, whose name later popped up on Lankford’s son’s iPad, kept the letters in their original envelopes and shared them with ProPublica. He said he never suspected Williams was doing anything illegal.
In his letters, Williams said that when he got out, instead of training clients himself, he would recruit clients and other trainers to run the sessions. “It has the potential for increased revenue.”
He asked Cosio to remove the term “personal training” from his website in another letter, adding “95 percent of my clients are paid for by insurance, which does not cover ‘personal training,’ I have to bill it as ‘therapeutic exercise.’ It is the same thing, but I have to play the insurance game … Insurance pays twice as much as cash pay so I have to go after that market.”
Williams downplayed his child abuse conviction—”I can honestly say that I am the only one in here for spanking their child”—and included a dig at his ex-father-in-law, Pratte: “an evil, evil man. He is the reason for my new accommodations.”
Williams told Cosio he needed to raise a quick $30,000 to pay an attorney to get him access to his children. “I will need to get a bunch of clients in a hurry.”
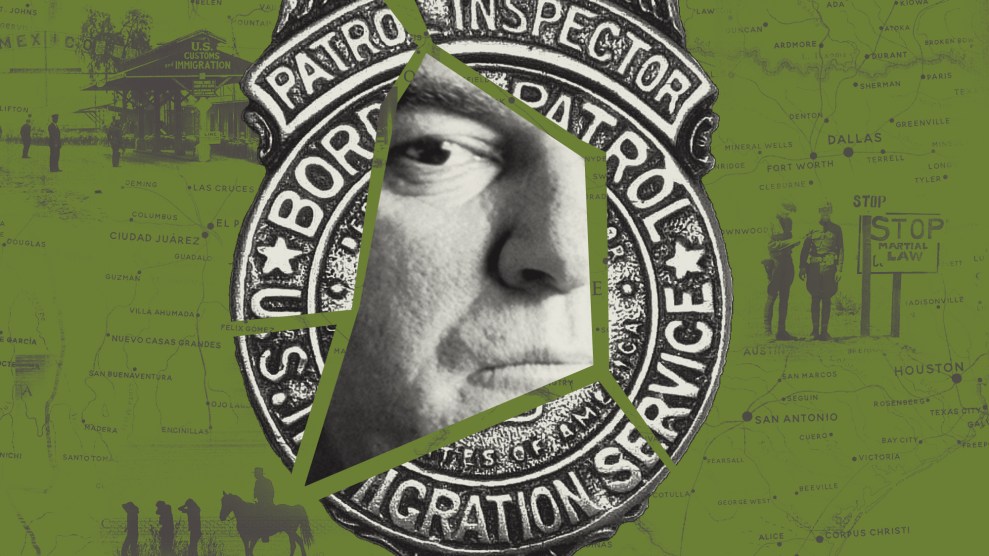
To set his plan in motion, Williams needed what is essentially the key that unlocks access to health care dollars: a National Provider Identifier, or NPI number.
The ID number is little known outside the medical community but getting one through the federal government’s Medicare program is a rite of passage for medical professionals and organizations. Without it, they can’t bill insurers for their services.
One would think obtaining an NPI, with its stamp of legitimacy, would entail at least some basic vetting. But Williams discovered and exploited an astonishing loophole: Medicare doesn’t check NPI applications for accuracy—a process that should take mere minutes or, if automated, a millisecond. Instead, as one federal prosecutor later noted in court, Medicare “relies on the honesty of applicants.”
Records show Williams first applied for an NPI under his own name as far back as 2008. But it wasn’t until 2014 that Williams began to ramp up his scheme, even though now he wasn’t just unlicensed, he was a two-time felon. He got a second NPI under the company name, Kinesiology Specialists. The following year, he picked up another under Mansfield Therapy Associates. In 2016, he obtained at least 11 more, often for entities he created in the areas where he found fitness clients: Dallas, Nevada, North Texas and more. By 2017, he had 20 NPIs, each allowing him a new stream of billings.
For every NPI application, Williams also obtained a new employer identification number, which is used for tax purposes. But he never hid who he was, using his real name, address, phone number and email address on the applications. He added the title “Dr.” and listed his credentials as “PhD.” Under medical specialty he often indicated he was a “sports medicine” doctor and provided a license number, even though he wasn’t a physician and didn’t have a medical license.
Medicare officials declined to be interviewed about Williams. But in a statement, they acknowledged that the agency doesn’t verify whether an NPI applicant is a medical provider or has a criminal history. The agency claims it would need “explicit authority” from the Department of Health and Human Services to do so—and currently doesn’t have it. Regulations, and potentially the law, would need to be revised to allow the agency to vet the applications, the statement said.
Medicare does verify the credentials of physicians and other medical providers who want to bill the agency for their Medicare patients.
To those charged with rooting out fraudsters, the current regulations seem like an invitation to plunder.
“Medicare has to make sure that the individuals who apply for NPIs are licensed physicians—it’s that simple,” said Elliott, the former prosecutor who ran about 100 health care fraud investigations.
Elliott, who now does white-collar criminal defense, said he knows of two other cases currently under federal investigation in which non-licensed clinic administrators lied to obtain NPI numbers, then used patients’ information to file false claims worth millions.
Medicare warns NPI applicants that submitting false information could lead to a $250,000 fine and five years in prison. But since Medicare started issuing NPIs in 2006, officials said they could not identify anyone who had been sanctioned.
So, for those bent on fraud, the first step is easy; the online approval for an NPI takes just minutes.
Williams got out of jail in November 2012 and launched an aggressive expansion with an irresistible pitch: Time to get those private personal training sessions you thought you couldn’t afford!
“Now accepting most health insurance plans,” his Get Fit With Dave website announced. He added a drop-down menu to his site, allowing potential clients to select their health insurance provider: Aetna. Blue Cross Blue Shield. United.
He began building a team, soliciting trainers from the strength and conditioning department at Texas Christian University. He met with new recruits at local fast food joints or coffee shops to set them up. To the trainers, the business appeared legit: They even signed tax forms. Before long, Williams’ network stretched throughout Texas and into Colorado, Idaho and Nevada.
One Fort Worth trainer recalled meeting Williams through one of his clients, a Southwest Airlines flight attendant. Williams, he said, seemed like a real doctor, and it wasn’t hard to imagine an insurer’s wellness program covering fitness. Plus, it was good money—about $50 an hour and Williams paid him for multiple clients at once if he did boot camps, said the trainer, who asked that his name not be used so he wouldn’t be tarnished by his association with Williams. Williams, he said, even gave him an iPad, with “Kinesiology Specialists” etched on the back, to submit bills and paid him via direct deposit.
Clients came to Williams through his business cards, his website and word-of-mouth. Williams, records show, quickly verified if their insurance companies would cover his fees—although he didn’t tell clients that those fees would be billed as medical services, not personal training. To ensure the clients paid nothing, he waived their annual deductibles—the portion patients pay each year before insurance kicks in. Authorities said Williams banked on being able to file enough claims to quickly blow through their deductibles so he could get paid.
Meredith Glavin, a flight attendant with Southwest, told the authorities she got in touch with Williams after her co-workers said insurance was covering their workouts. After providing her name, address and insurance information on the Get Fit With Dave website, Williams emailed back with the good news: “Everything checks out with your insurance. My services will be covered at no cost to you.”
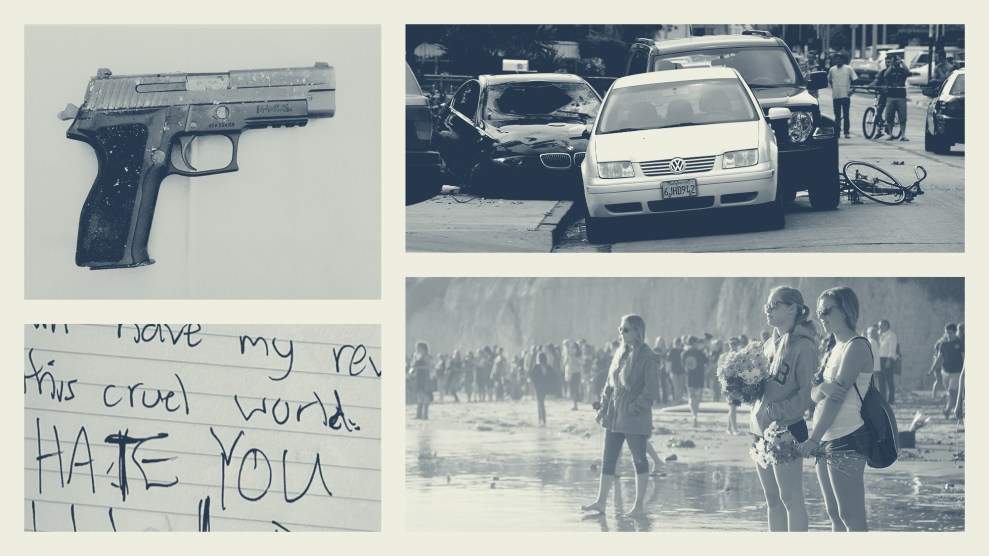
During a follow-up phone call, Glavin said, they discussed her fitness and weight loss goals and then Williams connected her with a trainer. The workouts were typical fitness exercises, she said, not treatment for a medical condition. But insurance claims show Williams billed the sessions as highly complex $300 examinations to treat “lumbago and sciatica,” a condition in which nerve pain radiates from the lower back into the legs.
He used his favorite billing code—99215—to bill Glavin’s insurer, United, the claims show. The code is supposed to be used less often because it requires a comprehensive examination and sophisticated medical decision-making, warranting higher reimbursement. In all, Williams used the code to bill United for more than $20.5 million—without apparently triggering any red flags at the insurer. For that code alone, the insurance giant rewarded him with $2.5 million in payments.
Eventually, Get Fit With Dave expanded to about a dozen trainers and around 1,000 patients, said a source familiar with the case. And, court records show, the checks from insurance companies, some over $100,000, kept rolling in.
Williams bought a couple of pick-up trucks, a new Harley Davidson motorcycle and a fancy house. But greed didn’t seem his only motivation. “I made $50K last week,” he wrote in a December 2014 text to a friend. “Seriously it means nothing. It is not about the money. I have had a lot taken away from me, and maybe I am trying to prove something … Maybe it is my way of giving the finger to everyone???”
A few miles away, his former father-in-law watched Williams’ illegal business blossom with growing outrage. Pratte kept his grandson’s iPad on his desk, near his computer, and checked it every day. The texts appeared boring, even routine, but Pratte knew they were evidence of ongoing fraud.
“I have another flight attendant friend who is interested in signing up as well,” a new client texted to Williams.
“Tell him to show up with his insurance card,” Williams replied.
To Pratte, the text messages were a “gold mine.” This is the stuff that will really nail his rear end, he recalled thinking as he read the messages. He couldn’t wait to share his findings with the insurers. How often do they get cases wrapped up in a bow?
But when he and Lankford began contacting insurers, they were soon bewildered. When Pratte told Aetna that he wanted to report a case of fraud, he said the customer service representative asked for his member number, then told him non-members couldn’t report criminal activity. Lankford, who happened to be covered by Aetna, made the complaint, but they say they never heard back.
An Aetna spokesman told ProPublica that the insurer could find no record of Pratte’s call but said the company’s fraud hotline takes tips from anyone, even anonymous callers.
Lankford sent an email to Cigna’s special investigations unit in January 2015 “regarding one of your providers that concerns me.” She provided Williams’ company name, address, cellphone number, Social Security number and more, and she described his scheme. “He has no medical license or credentials,” she wrote. “He was in prison for felony theft.”
A supervisory investigator called to ask for the names of personal trainers, which Lankford provided. But, again, there was silence.
Pratte could see many of the clients worked for Southwest and had their benefits administered by United. He jotted down the name, address, phone number, birthdate and member identification number of the potential clients on a yellow legal pad—all the information the insurer and Southwest would need to investigate the fraud. This is so easy, Pratte recalled thinking as he wrote down the details, all they have to do is cross-reference this.
Because Southwest self-funds its benefits, the company was on the hook for the bills, which would eventually total about $2.1 million according to a source familiar with the case. It paid United to administer the company’s plan and ensure the claims it covered were legitimate. Pratte said he called the airline in the fall of 2015 and spoke to someone in the human resources department who said they would pass the information to the right people. “That was the last I heard,” he said. Southwest declined to comment for this story. It still pays United to administer its benefits.
Pratte started calling United in the fall of 2014 and spoke to a fraud investigator who took the information with interest, he said. But within a couple of weeks he was told she moved to a different position. Pratte continued calling United over the following two years, making about a dozen calls in total, he said. “He is not a doctor,” Pratte told whoever picked up the phone. “So, I don’t see how he can be filing claims.”
In early 2015, Lankford emailed additional information to the investigator. The investigator wrote back, thanking Lankford and saying she forwarded the details to the people who research licenses. “They will investigate further,” she said in the email.
Meanwhile, the text messages showed Williams continuing to sign up—and bill for—United members.
Frustrated, Pratte made one final call to United in 2016, but he was told the case was closed. United said he’d have to call the Texas Department of Insurance for any additional details. Pratte had already filed a complaint with the regulator but reached out again. The department told him that because he hadn’t personally been defrauded, it would not be able to act on his complaint.
To Pratte, it appeared he had struck out with Aetna, United, Southwest and the Texas Department of Insurance. “I was trying to get as many people as possible to look into it as I could,” Pratte said recently. “I don’t know if that tells me they are incompetent. Or they don’t care. Or they’re too busy.”
A case summary, prepared by the Texas Department of Insurance, shows it first learned of the Williams case in January 2015 but lacked staff to investigate. A spokesman said the regulator later received Pratte’s complaint but didn’t pursue it after learning that United had already investigated and closed its case.
Meanwhile, some Get Fit With Dave clients had begun noticing odd claims on their insurance statements.
Nanette Bishop had heard about Williams when a fellow Southwest flight attendant handed her the trainer’s business card and said, “You’ve got to meet Dr. Dave.” (Bishop said the Southwest legal department advised her not to speak with ProPublica. Details about her interaction with Williams come from court records.)
Bishop said she started strong with the workouts but “fizzled” quickly. Her daughter, who was also on her plan and signed up for workouts, only did a couple sessions. Bishop said she had a hard time staying consistent because she was traveling a lot—for much of October 2014 she was in Germany. Later, she noticed in her insurance records that Williams had been paid for dozens of sessions over many months, even during the time she’d been abroad.
Bishop texted Williams in January 2015 to tell him he needed to refund all the money. “I never worked out four [times] a week and [my daughter] quit the first week of September,” she wrote. Bishop also called United and Southwest Airlines to report the overbilling.
About a month later, Williams received a letter from a subsidiary of United ordering a review Bishop’s medical records.
Another client texted Williams with concerns that her United insurance plan had been billed for 18 workouts in December 2015. That couldn’t be accurate, the woman wrote. “I had to take December off due to my work schedule and family in town,” she wrote. “I understand that people need to be paid but this seems excessive.”
While Pratte, Lankford and some of Williams’ clients repeatedly flagged bogus bills, the mammoth health insurers reacted with sloth-like urgency to the warnings. Their correspondence shows an almost palpable disinterest in taking decisive action—even while acknowledging Williams was fraudulently billing them.
Cigna appears to have been the quickest to intervene. In January 2015, Cigna sent Williams a letter, noting that he wasn’t a licensed medical provider and had misrepresented the services he provided. The insurer said he needed to pay back $175,528 and would not be allowed to continue billing.
“I just got a $175K bill in the mail,” Williams texted to a friend. “Cigna insurance has been overpaying me for the past 18 months and they want it back. I knew that they were reimbursing at too high of a rate so I can’t really complain.”
By then Williams had more than one National Provider Identifier, so he just switched numbers and kept billing Cigna. More than a year later, in May 2016, Cigna sent another letter, saying he now owed $310,309 for inappropriate payments. In total, the company paid him more than $323,000. Williams never gave any of it back. Cigna declined to comment about the Williams case.
Aetna wrote Williams in January 2015 to say it had reviewed his claims and found he wasn’t licensed, resulting in an overpayment of $337,933. The letter said there appeared to be “abusive billing” that gave “rise to a reasonable suspicion of fraud.” But the insurer also gave him a month to provide documentation to dispute the assessment. When Williams hadn’t responded in three months, an Aetna investigator wrote to Williams’ attorney, saying, “We are willing to discuss an amicable resolution of this matter,” and gave him two more weeks to respond.
That August, an Aetna attorney sent Williams’ attorney another letter, noting that Williams had submitted “fraudulent claims” and had continued to submit bills “even after his billing misconduct was identified.”
In January 2016—a year after Aetna first contacted him—Williams agreed to a settlement that required him to refund the company $240,000 “without admission of fault or liability by either party.”
But that didn’t stop, or even appear to slow, Williams. Not only did he renege on that promise, he picked one of his other NPI numbers and continued to file claims resulting in another $300,000 in payments from Aetna. In total, Aetna paid Williams more than $608,000.
In emails, Ethan Slavin, a company spokesman, didn’t explain why Aetna settled with Williams instead of pursuing criminal prosecution. He blamed the insurer’s slow response on the lengthy settlement process and Williams’ tactic of billing under different organizations and tax identification numbers. Williams did repay some of the money before defaulting, Slavin said.
United, one of the largest companies in the country, paid out the most to Williams. The insurer brought in $226 billion last year and has a subsidiary, Optum, devoted to digging out fraud, even for other insurers. But that prowess is not reflected in its dealings with Williams.
In September 2015, United wrote to Williams, noting his lack of a license and the resulting wrongful payments, totaling $636,637. But then the insurer added a baffling condition: If Williams didn’t respond, United would pay itself back out of his “future payments.” So while demanding repayment because Williams was not a doctor, the company warned it would dock future claims he would be making as a doctor.
Williams responded a month later, noting that he had a Ph.D. in kinesiology and did rehab, so he met the qualifications of a sports medicine doctor.
United responded in November 2015 with the same argument: he wasn’t licensed and thus needed to repay the money, again warning that if he didn’t, United would “initiate repayment by offsetting future payments.”
Williams took United up on its offer. “Please offset future payments until the requested refund amount is met,” he responded.
Then Williams turned to another NPI number, records show, and continued submitting claims to United.
In January 2016, Williams agreed to settle with United and repay $630,000 in monthly installments of $10,000. Inexplicably, the agreement refers to Williams as “a provider of medical services or products licensed as appropriate under the laws of the state of TX” and notes that the settlement doesn’t terminate his continued participation in United’s programs.
In 2016, Williams obtained a new batch of NPI numbers from Medicare. As usual, he used his real name, address and credentials on the applications. The additional numbers allowed him to continue to make claims to United.
In November 2016, United investigators caught Williams again—twice. They sent two letters accusing him of filing 820 claims between May 2016 and August 2016 and demanded repayment. Again, almost inconceivably, the company threatened to cover his debt with “future payments.”
In December 2016, United notified Williams he had only repaid $90,000 of the initial $630,000 he owed and was in default. The following month, United told him he had to pay the remaining $540,000 within 20 days or he could face legal action. Williams replied, saying he wanted to renegotiate the settlement, but the insurer declined. Late that month, United said its inappropriate payments to Williams had ballooned to more than $2.3 million.
A United spokeswoman said it was difficult to stop Williams because he used variations on his name and different organizations to perpetrate the fraud. “He did everything he could not to get caught,” Maria Gordon-Shydlo said.
She acknowledged getting the complaints from Lankford and Pratte, as well as United members, but defended the response of the company, saying it had eventually referred Williams to law enforcement.
The insurer is continuing “to improve our processes and enhance our systems so we can catch these schemes on the front-end,” she said, “before a claim is paid and to recoup dollars that were paid as a result of provider misconduct.”
In all, United paid Williams more than $3.2 million—most of it after the insurer had caught him in the act.
But in reality, the losses weren’t all United’s. Most of the fraud was funded by its client, Southwest.
Many health care experts and fraud investigators said they weren’t surprised to hear that insurers were slow to stop even such an outlandish case of fraud.
“It’s just not worth it to them,” said Dr. Eric Bricker, an internist who spent years running a company that advised employers who self-funded their insurance.
For insurance behemoths pulling in billions, or hundreds of billions, in revenue, fraud that sucks away mere millions is not even a rounding error, he said.
And perhaps counterintuitively, insurance companies are loath to offend physicians and hospitals in their all-important networks—even those accused of wrongdoing, many experts have said. They attract new clients by providing access to their networks.
This ambivalence toward fraud, Bricker and others said, is no secret. Scammers like Williams are “emblematic of gazillions of people doing variants of the same thing,” Bricker said. Insurers embolden them by using a catch-and-release approach to fraud, in which the insurers identify criminals, then let them go.
Joe Christensen has pursued fraud for both government and commercial insurers, serving as a director in Aetna’s Special Investigations Unit, a team of more than 100 people ferreting out fraud, from 2013 to 2018 and as the director of Utah’s insurance fraud division for 13 years. Fraud in government programs, like Medicare and Medicaid, gets more publicity, he said, and has dedicated arms of agencies pursuing fraudsters. But the losses may be even greater in the commercial market because the dollar levels are higher, he said.
Some commercial insurers take a passive approach, Christensen said, in part because it’s expensive to press a fraud case. At Aetna, he said, investigators would identify cases of apparent fraud, but it was up to the executives and legal team to decide how to handle them. Taking fraudsters to civil or criminal court requires resources, so the company often settled for trying to get repaid through settlements or blocking a suspect provider from billing, he said.
Christensen said while he was at Aetna, investigators almost never sought to partner with law enforcement agencies to pursue criminal cases. Last spring, he became the SIU director for a Southern California-based Medicaid plan called L.A. Care Health Plan, where he was allowed to take a proactive approach. In just about a year, he said, his much smaller team began 37 criminal investigations with law enforcement agencies. The cases are in different stages, but so far there have been seven arrests, four search warrants and one conviction. Christensen recently took a job with an insurer in Utah, where his family lives, so he could be closer to them.
ProPublica asked Aetna how many criminal cases it had pursued in 2017 and 2018. A company official said the question could not be answered because it does not track such cases.
In the spring of 2017, more than four years after Williams first began billing insurers, one of them, United, finally brought him to the attention of the FBI’s heath care fraud squad.
One May day, agents from the FBI and the newly engaged Texas Department of Insurance knocked on the door of Williams’ sprawling six-bedroom home—a spread he’d boasted to one trainer that he’d purchased with cash. Williams didn’t invite them in. He refused to answer questions, claiming his attorney had dealt with the questionable billings.
Undaunted, just days later, Williams used a freshly minted NPI number to send another bill to United. The last known claim he submitted was on June 3, 2017, according to a source familiar with the investigation.
That October, Williams’ long run came to an end when he was arrested by the FBI.
The following May, Williams’ trial began in the United States District Court for the Northern District of Texas. The prosecution didn’t have to make a complex argument. Williams had billed for non-medically necessary services and wasn’t a medical provider—a “slam dunk case” said the agent on the case.
But the testimony served as a cheat sheet for how to defraud the health insurance industry and mostly get away with it.
Without irony, the prosecutor, P.J. Meitl, argued that Williams had preyed on a health insurance system that relies “on trust, relies on honesty” when it pays claims.
He called fraud investigators from Aetna, Cigna and United, who testified that their companies auto-pay millions of claims a year. It’s not cost effective to check them, they said. “Aetna relies on the honesty of the person submitting the claim verifying that it’s true,” testified Kathy Richer, a supervisor in Aetna’s Special Investigations Unit.
In a similar manner, Medicare trusts that people who apply for NPI numbers are actually medical providers, Meitl told the jury. Medicare “does not investigate or verify whether an individual is actually a health care provider before issuing an NPI number.”
Williams’ attorney, Wes Ball, argued that the case was the sign of a “broken” health care system and blamed insurers for making a financial decision not to review Williams’ claims before paying them. United failed to protect Southwest’s money, Ball said, and “might be a vendor you might not want to hire.”
As for the NPI numbers, anyone could have checked Williams’ credentials, he said.
The jury wasn’t convinced, convicting Williams of four counts of health care fraud.
The judge sentenced him to a little more than nine years in federal prison and ordered him to pay $3.9 million in restitution to United, Aetna and Cigna.
Insurers promote themselves as guardians of health care dollars. United says on its website it wants to “help employers manage” medical expenses, resulting in “lower costs.” Aetna promises employers “affordability.” Cigna promises “increased savings.”
But private health insurers allow so much fraud that prosecutors use an idiom to describe the rare person who gets caught: “Pigs get fat, hogs get slaughtered.”
“Pigs” can steal millions, if they bill just enough to avoid notice. But if they get greedy and bill too many millions, they “become a data outlier,” said Elliott, the former fraud task force prosecutor. “You get slaughtered.”
Williams took years to reach hog status.
Part of the problem, experts say, is that health care fraud is often misunderstood as shafting greedy insurers—not the folks paying for health insurance. Ultimately, insurers don’t bear the cost. For their self-funded clients, like Southwest, they merely process the claims. For their traditionally insured clients, they can recover any losses by increasing deductibles and premiums and decreasing coverage.
Williams appears to have duped more than insurers. His twin brother, Dan Williams, recently retired as the assistant special agent in charge of the Dallas field office for criminal investigation for the Internal Revenue Service. He spent 27 years ferreting out fraud, and he gets the irony. “You’re not the first person to point that out,” he said.
Dan Williams said his brother’s sudden riches from the training business piqued his investigative instincts, but he “trusted” his brother when “he told me he was authorized to bill insurance companies.”
In his letter to ProPublica, Williams did not address the issues in the case or even acknowledge that any of his activities were wrong. Instead, he blamed his former wife.
“It grieves me that the consequences of a bitter and hurtful divorce have resulted in the ending of this unprecedented and beneficial opportunity to help many people,” he wrote.
Lankford and Pratte are proud of their part in ending his scheme, if still baffled that they had to play such a central role in uncovering it.
If it hadn’t been for the iPad messages, “I have to believe he would still be billing insurance companies from a Caribbean island,” Pratte said.