<a href="http://www.shutterstock.com/pic-158810372/stock-photo-a-pile-of-chicken-nuggets-isolated-on-a-white-background.html?src=EwZvM4O4f30MHg_UfkheTQ-1-25" target="_blank">dolphfyn</a>/Shutterstock
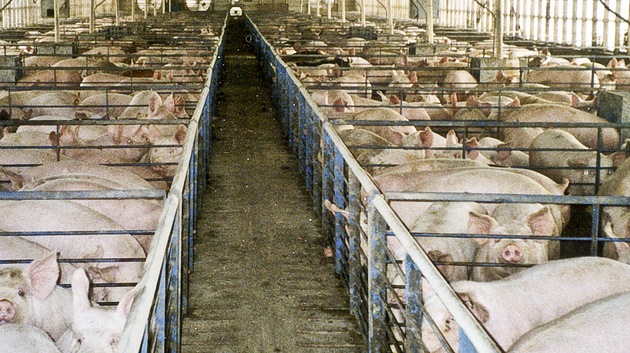
Last week, the FDA released a report on the gross amount of antibiotics purchased by the livestock industry in 2012. The results are a bit startling. Between 2009 and 2012—a period of increasing awareness about the perils of antibiotic use in livestock facilities—the FDA found purchases of the drugs rose 16 percent. Over the same period, annual production of beef, chicken, and pork barely budged, suggesting that the industry was becoming more antibiotic-intensive each year. Worse still, the FDA deemed 61 percent of the antibiotics sold to the meat industry in 2012 as “medically important”—meaning that they’re commonly used in human medicine, and thus in danger of losing their effectiveness through resistance.
Late last year, after decades of foot shuffling, the FDA made its most decisive attempt ever to tamp down the meat industry’s habit of dosing livestock with antibiotics to make them grow faster—although being a rather timid watchdog, the FDA chose to make the rules voluntary.
The new report shows just how dire things had become: 70 percent of the “medically important” antimicrobials sold to meat producers in 2012 were destined to be administered through feed, and another 24 percent through water. Just 6 percent were meant to be used topically or through injection—the way small-scale farmers use antibiotics to treat sick animals. “If you talk to a veterinarian, they’ll tell you that if drugs are being used in feed, for the most part, they’re being used to promote growth or prevent disease, not to treat an animal that’s known to be sick,” Keeve Nachman, who directs the Food Production and Public Health Program at Johns Hopkins’ Center for a Liveable Future, told me. Also, 97 percent of the drugs were sold without a prescription from a veterinarian—a practice that the 2013 rules intend to stop.
Even worse, as Keeve Nachman pointed out, sales of cephalosporins, a drug used to treat respiratory-tract infections, skin infections, and urinary-tract infections in people, rose about 4 percent between 2011 and 2012, even though the FDA had moved to scale back their use on January 4, 2012. That doesn’t exactly boost confidence.
Before I could fully digest this data, another email arrived in my inbox, this one from the meat-industry trade paper WATT Agribusiness, to which I subscribe. It contained an article sponsored by the ag-pharmaceutical giant Zoetis, titled “How do antibiotics promote growth?”
The piece suggests that Zoetis is still marketing antibiotics as a way to make animals grow faster, while staying within the bounds of the FDA’s voluntary restrictions on using “medically important” drugs for that purpose. The piece cites an antibiotic called bacitracin, which the FDA considers “not currently medically important,” as something farmers should consider for growth-promotion purposes.
According to Steven Roach, a senior analyst at the group Keep Antibiotics Working, there are two problems with this approach. First, “not everyone agrees that bacitracin is not medically important,” he said. While the FDA doesn’t currently list it as important, it hasn’t reevaluated its “medically important” list since 2003, he said. Meanwhile, bacitracin is used in human medicine, most commonly as an ointment to prevent infection in minor cuts, scrapes, and burns. And the World Health Organization lists it as an “important antimicrobial for human medicine.”
Widespread use in livestock facilities could make it ineffective for current uses—and eliminate the prospects for future treatments that could be developed from it.
The second problem, he said, is that the heavy use of antibiotics that are really not used in human medicine can cause harm through cross-resistance—that is, bacteria strains that develop resistance to one antibiotic can quickly become resistant to others.
Cross-resistance is a well-established phenomenon. Johns Hopkins’ Nachman explained cross-resistance like this: Antibiotic resistance occurs when bacteria evolve to survive contact with a chemical intended to kill them. And “in teaching bacteria to survive in the presence of a [non-medically important] drug, we may also be teaching them how to survive in the presence of a drug we do rely on,” he said.
Nachman says a shift to non-“medically important” drugs is certainly preferable to the status quo, but won’t likely fully solve that our factory farms are now incubating resistant bacteria strains that threaten people.