A few days ago I wrote a post about the rise in maternal mortality in America, and in particular the stunning difference between black and white mothers in the rate of maternal death. Using a back-of-the-envelope look at patterns of racial bias vs. racial differences in maternal mortality, I found little reason to think that racism among delivery doctors was the likely cause of this. I got some pushback about this on Twitter, mostly saying that the delivery room was too narrow a focus. At the very least I needed to look at the entirety of prenatal care, and beyond that the differences in black-white lifetime medical care.
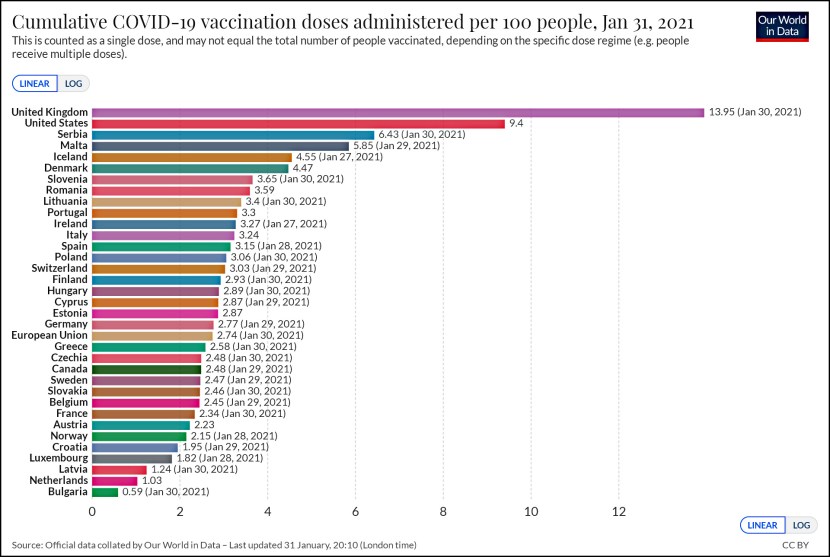
That was fair enough, so I decided to look into this. Fair warning: this post is longish and chart-tastic and doesn’t come to any firm conclusions. Read on at your own risk. To start, here’s the basic problem we’re dealing with:
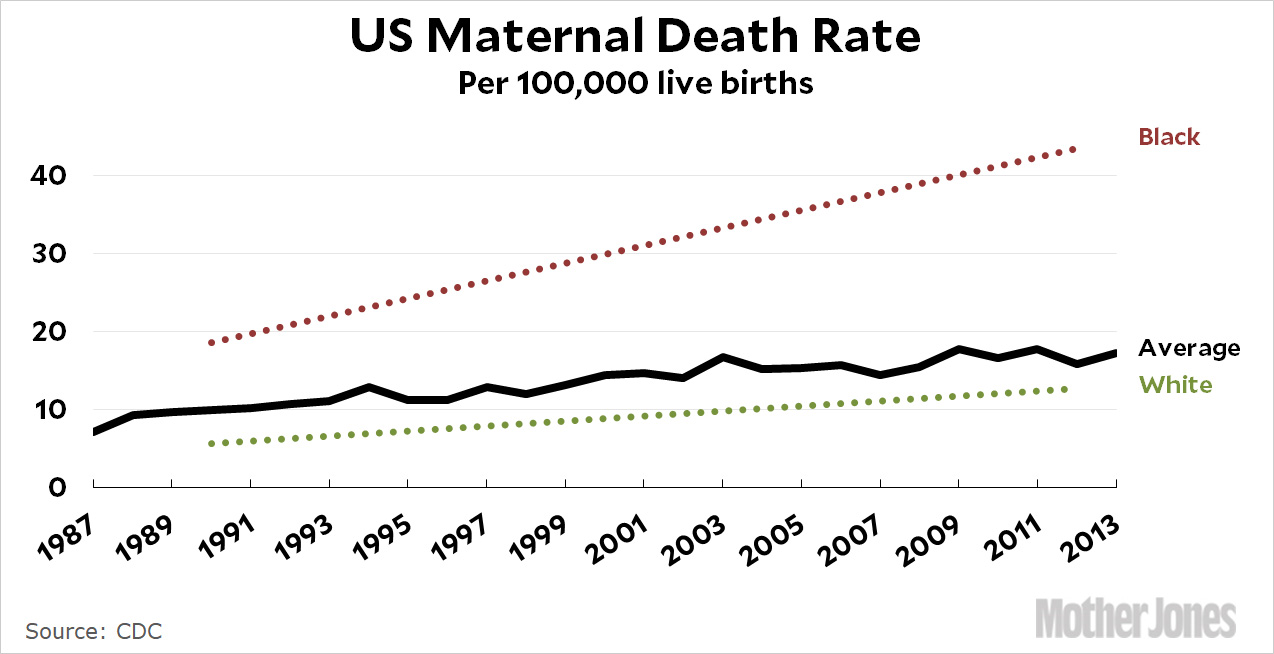
Not only is the maternal mortality rate going up, but the difference between black and white mothers has been widening. Nor is this something that’s been recognized only recently: there are papers going back more than 20 years on the subject. That said, there are shockingly few rigorous studies trying to tease out the causes of this disparity. Last year, for example, the New York Times Magazine published a long article about black maternal mortality written by Linda Villarosa, a journalist who’s been following the subject for many years:
The reasons for the black-white divide in both infant and maternal mortality have been debated by researchers and doctors for more than two decades. But recently there has been growing acceptance of what has largely been, for the medical establishment, a shocking idea: For black women in America, an inescapable atmosphere of societal and systemic racism can create a kind of toxic physiological stress, resulting in conditions — including hypertension and pre-eclampsia — that lead directly to higher rates of infant and maternal death. And that societal racism is further expressed in a pervasive, longstanding racial bias in health care — including the dismissal of legitimate concerns and symptoms — that can help explain poor birth outcomes even in the case of black women with the most advantages.
“Growing acceptance” is correct, and the toxic stress hypothesis is intuitively appealing. It’s also theoretically appealing, since there are known pathways for stress to affect pregnancy and childbirth. But for all its length, the article provides no real evidence for it. One reason for this is the “Hispanic paradox”: Hispanics certainly encounter systemic racism too, but the maternal mortality rate for Hispanic mothers is about the same as for white mothers.
Consider the following chart. It comes from a study that measured the average “allostatic load” for blacks, whites, and Hispanics. There’s no firmly accepted definition of allostatic load, but generally speaking it’s a combination of factors like high blood pressure, high cholesterol, and inflammation that are thought to be strongly influenced by long-term stress. The problem is that if you accept both the AL theory and the toxic stress hypothesis, they don’t seem to correlate well. Here are results from a large-scale study using NHANES data:
The differences in allostatic load are tiny—about the equivalent of one IQ point on an intelligence test—and Hispanics have a higher allostatic load than either blacks or whites but the lowest maternal mortality rate. Note that although this is highly suggestive, it’s still a comparison of groups, so it doesn’t prove anything firmly. What you’d really like to see is a study that measures allostatic load in individuals during pregnancy and then analyzes whether it’s predictive of later maternal mortality. But that study doesn’t seem to exist.
However, there are multiple studies confirming that racial differences in allostatic load are small. One study—also with large sample sizes—reviewed three different measures of allostatic load. Using standard deviations to normalize them, the three measures showed that blacks had a mean allostatic load that was 0.1, 0.2, and 0.29 SDs higher than whites. Taking the average, this suggests that blacks have an AL about 0.2 SDs higher than whites—roughly the equivalent of three IQ points. A third study, unfortunately, doesn’t report standard deviations, but the results that were reported are consistent with a black-white difference of perhaps one-quarter of a standard deviation. Taken together, then, the black-white difference in allostatic load appears to be the equivalent of 1-3 points on an IQ test. That’s barely enough to be noticeable.
Finally, a fourth study in New Orleans found that black mothers had a lower allostatic load than white mothers. This result is probably a fluke, but it’s consistent with the other studies, all of which showed that racial differences in allostatic load are quite small.
What about other measures of stress? They’re hard to come by, but Arline Geronimus, who originated the “weathering” theory to explain black-white differences, has studied the length of telomeres in black and white women. Telomeres are the stabilizing caps on chromosomes, which shorten with age. Geronimus found that in middle-aged women, the telomeres in black women suggested an “age” about 7.5 years higher than in white women. It’s impossible to say what this means about the telomeres in younger women, but certainly the aging difference would be less, perhaps 2-3 years at most. Again, this suggests a fairly small difference between black and white women.
Perhaps even more puzzling for the toxic stress hypothesis, self-reported stress among the poor is lower for blacks than for whites:
Poor blacks report less stress and higher levels of optimism than both poor whites and poor Hispanics. Put all this together and the toxic stress/weathering hypotheses look shaky. The racial differences are modest and don’t seem to correlate well with maternal mortality anyway. The problem is that every other hypothesis seems wrong too. Researchers have looked at poverty, education, drinking, smoking, and genetic causes. None of them appear to be the answer. Highly-educated black women, for example, experience maternal mortality at much higher levels than highly-educated white women. So lack of education isn’t the cause. Another possibility is the timing of prenatal care, which differs moderately between black and white mothers, but studies suggest that it doesn’t explain the difference in maternal mortality either.
This mystery is what makes the toxic stress hypothesis appealing: it seems reasonable, since black women of all incomes and education experience stressful incidents of racism throughout their lives, and nothing else seems to account for their higher rate of maternal mortality. But if toxic stress turns out not to be the answer, what is? The first thing to look at is the causes of maternal mortality:
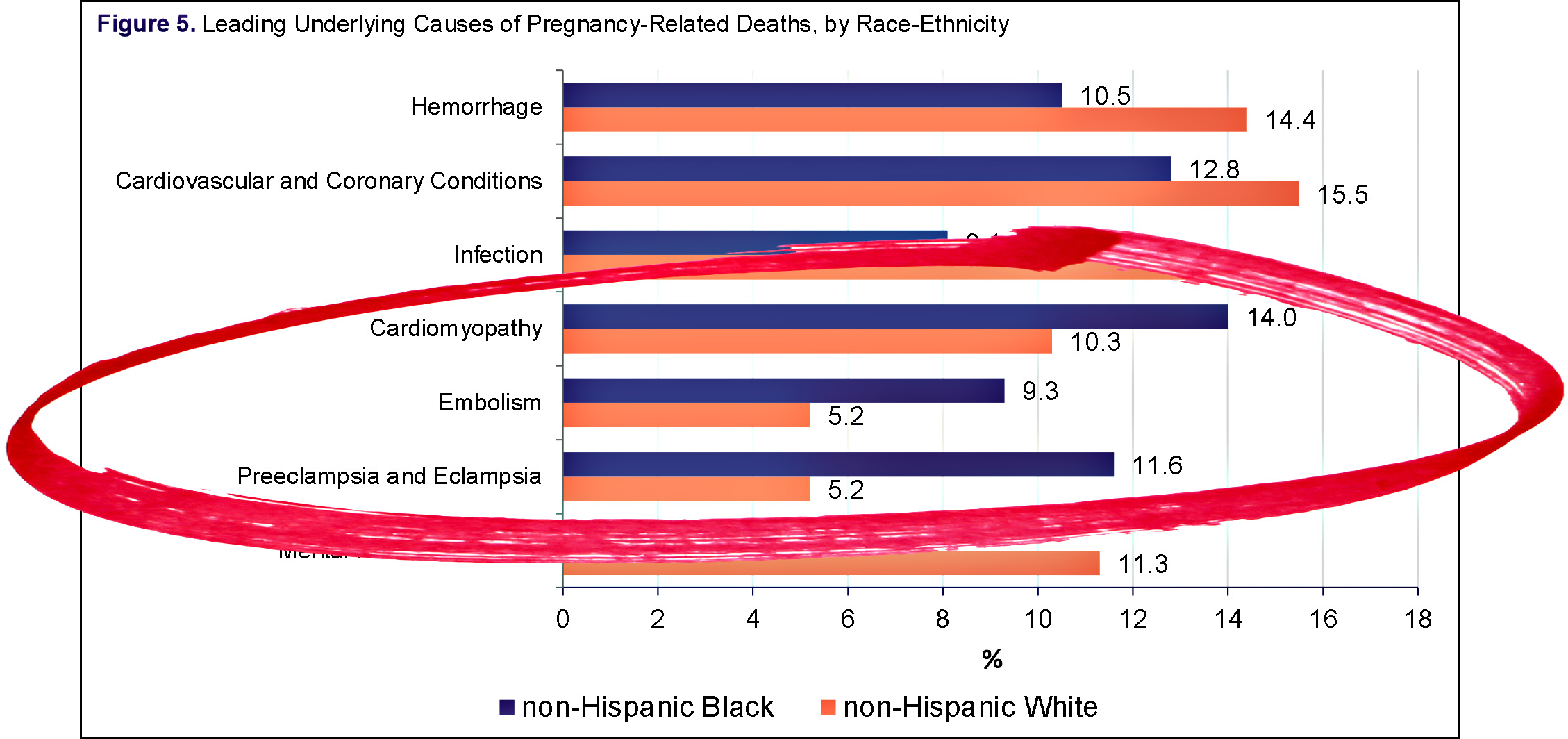
The three causes with the biggest black-white differences are cardiomyopathy (heart disease), embolism (blood clots), and eclampsia (a pregnancy-related illness that produces swelling and high blood pressure). All of these are related to the circulatory system. We can also look at black-white differences in diagnostic indicators during and after delivery. The following chart from a CDC study is complicated, so take a look at it and then read the explanation:
In this study, the researchers grouped hospitals as those that primarily served whites and those that primarily served blacks. The question is, are there differences in how black mothers are treated or diagnosed depending on the type of hospital? As you can see, the black-white differences (black bars) are fairly small for most indicators. They’re truly large only for two: PCD (problems with blood vessels in the brain during the six weeks following delivery) and IHM, or in-hospital mortality
The reasons for both of these are unclear. The white hospitals, in general, provided better care, but it’s not obvious why they’d diagnose post-delivery cerebrovascular disorders in black mothers so much more often than black hospitals. Is it because of a genuine difference, or simply due to better diagnostics?
Then there’s the startlingly high in-hospital mortality rate in white hospitals vs. black hospitals. However, this isn’t about the general fact that black mothers die at higher rates than white mothers. We already know that. What it seems to tell us is that there’s a difference in when black mothers die. Any pregnancy-related death within a year of delivery is counted as maternal mortality, and the difference in IHM rates suggests that in white hospitals black mothers die at high rates in the hospital, while in black hospitals they die at high rates after going home.
What we’re left with is this: Poverty, education level, drinking, smoking, and genetic causes don’t seem to explain the black-white difference in maternal mortality. The timing of prenatal care doesn’t explain it. Medically, the cause of the difference appears to be related to the circulatory system, which is sensitive to stress. This makes the toxic stress hypothesis intuitively appealing, but it has little rigorous evidence supporting it. There’s some modest evidence that wider use of doulas could reduce both infant and maternal mortality, but no evidence that it would reduce the black-white gap.
This is shocking: we still have almost no idea of what’s going on even though this has been a well-known problem for more than two decades. Even California, which has cut its maternal mortality rate in half over the past ten years—mostly by reducing the use of cesarian sections—has cut it equally for both black and white mothers. The enormous difference in black-white maternal mortality persists even in the state with by far the most success at addressing it.¹
But there’s finally some good news on this front. The reason we know so little is that there’s hardly any funding for research into the causes and prevention of maternal mortality. That changed a few months ago when Congress passed a bill that authorizes $58 million per year for the next four years to study maternal mortality. Hopefully a portion of this funding will be used specifically to study the black-white gap. For example, instead of looking at group differences in stress as measured by allostatic load—which is cheap but tricky to do right—we really need a study that measures allostatic load in individuals during pregnancy and then analyzes whether it’s predictive of later maternal mortality. With any luck, that’s the kind of study we’ll now be able to conduct.
¹California has recently added a specific program to look into the black-white gap, but it’s fairly new and hasn’t yet produced any results.