The numbers are now frighteningly familiar: Last year more than 100,000 people died of drug overdoses, bringing the total death toll to more than 1 million since the invention of OxyContin in 1996. By 2030 another million people are projected to die. Americans are more likely to die of an accidental drug overdose—especially when it involves fentanyl, a synthetic opioid 50 to 100 times stronger than heroin and surreptitiously laced into other drugs—than in a car accident.
But cars would kill 15,000 more people a year were it not for seatbelts. Seatbelts, helmet laws, and air bags are harm reduction strategies. They reduce the negative consequences of risky behavior.
For decades, drug policy experts have recommended that we embrace the seatbelts of drug use: overdose-reversing medicine like naloxone, kits that make it easy to test drugs for fentanyl, and clean needles that reduce the spread of deadly diseases associated with intravenous drug use, like HIV and hepatitis C. Joe Biden is the first president to embrace harm reduction as an essential part of the nation’s drug policy. As part of the American Rescue Plan, he put $30 million to “support community-based overdose prevention programs, syringe services programs, and other harm reduction services.” In May the Department of Health and Human Services promised $1.5 billion for state and local initiatives, including harm reduction, to combat addiction.

Volunteers practice injecting an overdose reversal drug into lemons.
Research shows that these strategies do help people survive. A 2018 study of national harm reduction policies found that opioid deaths dropped by 14 percent in states that made naloxone (also known by its brand name, Narcan) easier to get. A Seattle study of people who used injection drugs found that new participants in a syringe exchange program were five times more likely to enter treatment than those who weren’t in the program. Harm reduction is an acknowledgment that, as Judith Feinberg, a West Virginia University professor of infectious diseases and behavioral medicine, says: “If you’re not breathing, you’re not going into recovery.”
Yet the promotion of anything other than complete abstinence has always been a hot-button issue. Many people worry that giving out needles will coddle people struggling with substance misuse or even lead to addiction (despite evidence it does not). Others fear that such programs will bring crime to their neighborhoods. Harm reduction became a flashpoint in the ’90s, when, scared that Democrats would get tagged for being soft on crime, Bill Clinton declined to overturn a ban on syringe exchange funding, a decision he later said he regretted.

At an encampment in West Virginia, Hillbilly says that when SOAR could hand out syringes, they would also help connect people to services. “It wasn’t all about giving out needles,” she says. “People don’t get that.”
But as the opioid crisis grew—and, notably, was mowing down white communities—even conservative drug warriors were more willing to try harm reduction. Take Mike Pence, who in 2015, as governor of Indiana, reluctantly approved the state’s first syringe exchange program to combat a sky-high HIV outbreak in Scott County. A sheriff begged him, Pence prayed on it, and the program went on to make a huge dent in the outbreak. Years later, a team of epidemiologists found that ending the program would increase HIV infections by nearly 60 percent. Nevertheless, in 2021, local officials voted to shutter it.
The decision was part of a resurgent backlash against harm reduction. North Carolina legislators last year proposed restrictions that would effectively end clean syringe services. Earlier this year, the only such program in Orange County, California, ceased operations when the city of Santa Ana revoked its permit. And efforts to overturn preexisting restrictions are stalling out. Currently, some 27 states either outlaw or otherwise criminalize syringe exchange.
The pandemic, and the resulting uptick in some crime‚ helped GOP strategists like Christopher Rufo, who already had weaponized false narratives about progressive ideas like critical race theory to great effect, realize that harm reduction offered them another front in the culture wars. Rufo’s 2020 essay in City Journal—which carefully conflates the particularly controversial strategy of safe injection sites, where people can use drugs under supervision in case of overdose, with harm reduction more broadly—helped provide an intellectual framework to old fears.
The panic really took off earlier this year, when the conservative Washington Free Beacon reported that the government would be using American Rescue Plan money to “fund the distribution of crack pipes to drug addicts.” Though glass pipe exchange is a solid harm reduction strategy—it encourages smoking instead of injecting, which is deadlier—the administration’s flat-footed response ignited a media firestorm. During the ensuing outrage, Sen. Joe Manchin (a Democrat from West Virginia, the state with the nation’s highest rate, by far, of fatal overdoses) joined with Republican Sen. Marco Rubio to introduce a bill reinstating the ban on the use of federal funds for syringe services—despite the fact that Republicans, led by Mitch McConnell, had pushed to remove the ban just six years before.

Every weekend, Ainsley Bryce, the executive director of Holler Harm Reduction, sets up a syringe exchange in the back parking lot of a Dollar General in North Carolina, where people seek help across state lines.
The harm reduction freak-out has now carried over into the midterms, becoming a crucial issue in the Pennsylvania senate race between Mehmet “Dr.” Oz and Lt. Gov. John Fetterman, with the Republican National Committee falsely claiming that Fetterman wants to legalize heroin. In August, California Gov. Gavin Newsom vetoed a bill to create the state’s first safe injection sites, saying that while he believed in harm reduction, he felt this particular idea needed more study. The decision was widely understood to be largely about fears that the issue wasn’t a good one for Democrats up for election, or Newsom’s own presidential ambitions.

Ashley Schneider and Kyle Evans stop by Bream, a Presbyterian church in Charleston, West Virginia, to get showers, coordinate methadone appointments, secure food stamps and receive clothing and a meal.
Against this backdrop, photographer Stacy Kranitz and I visited hard-hit communities in Central Appalachia to document three different efforts—a nonprofit health fair, a medical clinic, and a scrappy DIY project—to save lives and change minds. We hoped to capture “the humanity and the generosity of spirit” that Feinberg says we all need to really understand the opioid crisis.

Charleston, West Virginia
Statewide overdose deaths 1999–2020: 11,387
“I hate to be corny,” says Jeff, “but love and connection definitely helps.” On a Tuesday evening in June, Jeff, a longtime heroin user, has joined a few dozen other Charleston residents at a Presbyterian church for the monthly mutual aid meeting held by Solutions Oriented Addiction Response. (Jeff’s name and the names of other people who use drugs have been changed.)

Every month, SOAR hosts a meeting in a local church where community members can pick up supplies and get trained on how to use naloxone.
SOAR distributes naloxone and provides training in administering it. It offers testing for hep C, referrals for medical care, and access to legal services. And at these monthly gatherings, it offers fellowship and food—and tonight, karaoke. But not syringes. Not anymore.
In 2018, the health department shut down the syringe exchange program it had operated since 2015. City officials cited the proliferation of discarded needles as the reason, but the program had been under steady attack by then-Mayor Danny Jones, a Republican who blamed it for everything from a rise in crime to declining city revenues.
SOAR stepped in, holding health fairs at which it gave out up to 1,000 units of naloxone, exchanged syringes, and offered HIV testing and treatment referrals. But in April of last year, West Virginia enacted legislation limiting the number of syringes SOAR can hand out and requiring clients to show ID. The city council followed with an ordinance imposing criminal charges for anyone violating the restrictions. Since many who attended the health fairs have no address or ID, SOAR ceased distributing syringes.

SOAR volunteers test clients for infections spread through injection drug use, like HIV, and offer other medical advice.
Data from testing at SOAR’s health fairs, where they continued to pass out other supplies, documented an uptick in HIV. The CDC deemed it “the most concerning HIV outbreak in the United States.” Warning that it could be “the tip of the iceberg,” the CDC released a set of recommendations to local officials, including “[m]eeting people who inject drugs where they are by reducing barriers to participation in harm reduction programs and bringing services to them through mobile and street outreach,” and using harm reduction programs to link people to other services, like mental health care, treatment for HIV, and rehab.
Without syringe exchange, HIV diagnoses continue to climb. But that’s not the only setback. When she was still able to hand out syringes, says Brooke Parker, who works for a federal HIV/AIDS program and is the vice president of SOAR’s board, “that’s how I got the majority of my targeted testing done.”
“I could go anywhere,” Parker says, “and say, ‘Hey, you need some supplies?’” Or “‘Here’s why I’m testing, and here’s why it’s important for you.’”
In her early days of outreach she tended to weird folks out; it was awkward. She was uncertain of how to most effectively approach people. She learned. “I started rolling up on people and saying, ‘Hey, you look like you have sex. You want some condoms?’” That got the conversation rolling.

“He was a character,” Betty Stemple says of her son, Andy Barefield, who died by overdose last year. “We called each other Charlie—’Charlie, can I get a cigarette?'” A memorial service was held for Barefield at Magic Island. Stemple had reached out to SOAR prior to his death. In the days after, her “SOAR sisters,” as Stemple calls them, were at her side. She is now part of an extended family.
The health fairs were designed to be a one-stop shop. But it was syringes that brought people in. SOAR’s co-director Joe Solomon says the county’s HIV task force seems uninterested in discussing how to pull these services together. And, Solomon notes, according to the West Virginia Center on Budget & Policy, the opioid crisis costs Kanawha County $30 million a week in treating hepatitis B and C, HIV, endocarditis, and neonatal abstinence syndrome, and in law enforcement and foster care. That’s the same amount Biden first allocated for harm reduction pilot programs.
So Solomon and a slate of other candidates are running for city council on a platform that includes building a 24-hour overdose prevention center and safe injection site, and an office of Recovery and Overdose Prevention led by and for people in recovery and people who use drugs.

Joe Solomon is the director of SOAR, a harm reduction nonprofit in Charleston, West Virginia, that was forced to end its needle exchange program. He is running for city council to gain more support for harm reduction initiatives in the government.
Meanwhile the SOAR team is working to assuage community fears about harm reduction. SOAR tripled the number of needle disposal boxes throughout the county just last year, Solomon says. “SOAR runs Appalachia’s largest drug-user-led syringe-cleanup crew.”
If they can change their neighbors’ perception of what they’re doing, maybe the attacks on public health will stop.

Knoxville, Tennessee
Statewide overdose deaths 1999–2020: 25,379
Today is Kiki’s 32nd birthday. It’s yet another blistering day in Knoxville, and scores of people are gathered under an I-40 overpass to escape the sun. Many, Kiki among them, used to camp here, but now law enforcement doesn’t allow it. The state of Tennessee has made it a felony to sleep overnight on public property. And like most everywhere in this region, in the country, there’s a severe shortage of affordable housing.
Kiki isn’t sure where she’ll sleep tonight, but she’s glad to see familiar faces from Choice Health Network’s harm reduction team. In the cool shade, she’s tested for hep C and chats with Lesly-Marie Buer, a harm reduction researcher and outreach worker.

Baby Girl is the furry companion of William and Melissa, who are visiting Choice’s Knoxville clinic to pick up syringes, Narcan, and a container in which they can safely dispose of used needles. The trio make the 50-minute drive once a week. It gets expensive, but William says they’ll continue coming. he is particularly worried that he might end up with fentanyl-laced drugs. “It pretty much takes your life every time you do it,” he says. “You have to use Narcan.”
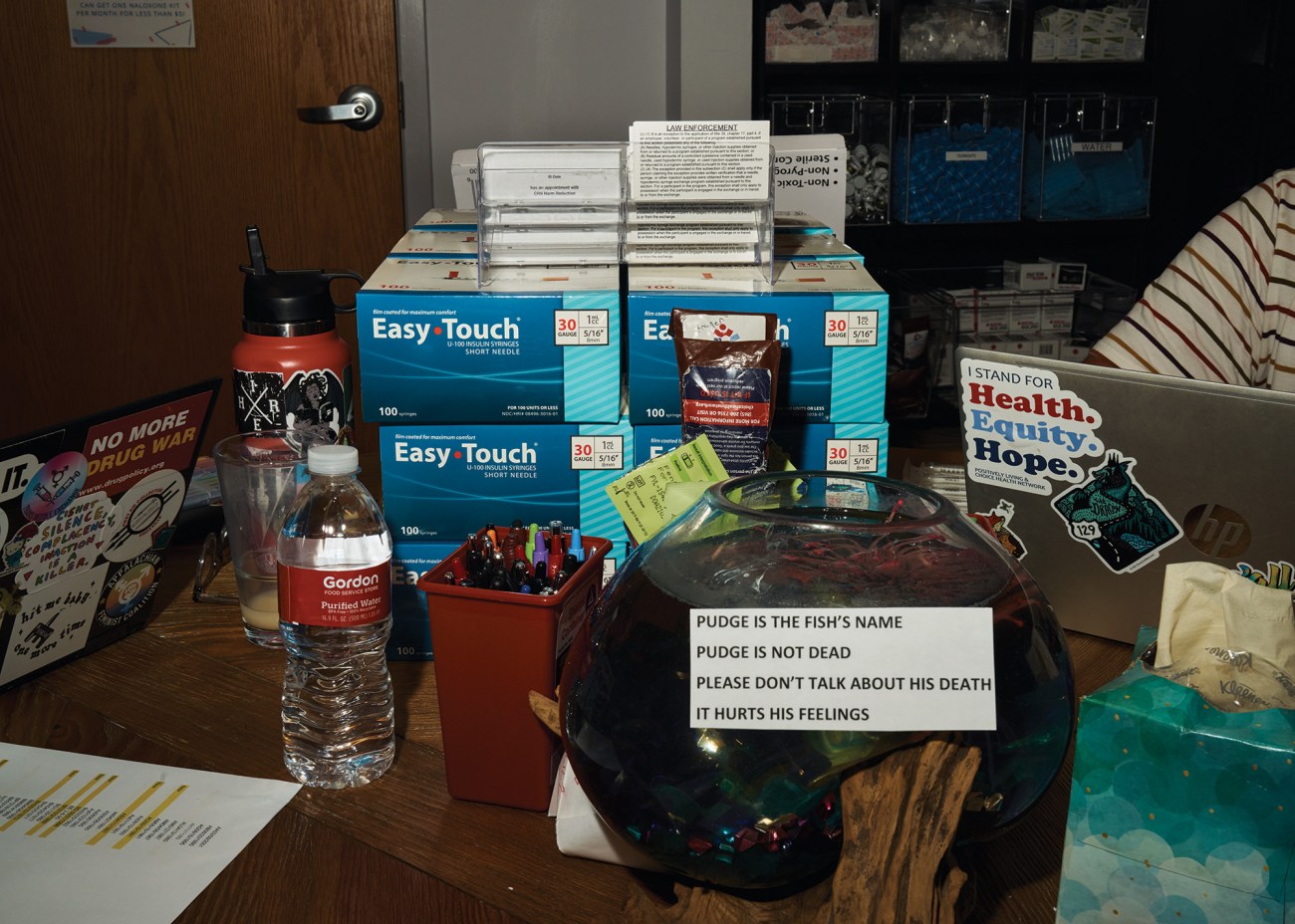
In addition to its outreach services, Choice hands out harm reduction supplies from its brick-and-mortar clinic.
Choice is a brick-and-mortar medical clinic that offers primary care for HIV patients, plus mental health counseling and harm reduction services. Every week, the team sets up a table of supplies under the overpass. Greg Stafford, Choice’s harm reduction medical coordinator, says their efforts are largely about education—things like basic wound care and the importance of rotating injection spots to avoid infection.
It’s also very much about building trust. “The unfortunate thing is that so many folks we serve have been treated poorly in social service or health care settings, or both,” says Genoa Clark, Choice’s harm reduction director. A primary objective is “making sure they feel seen and heard.” Many health care providers make assumptions that people who use drugs or are unhoused don’t value their health. Choice’s providers do not.

Choice’s harm reduction director picks up used syringes found at the underpass encampment.
If a person tests positive for HIV, they’re immediately connected with a case manager who helps launch treatment and assists with emergency housing, medical case management, and food and gas cards.
Local laws make their jobs difficult. State-certified needle exchange was legalized in Tennessee in 2018, but only a handful of programs yet exist, and it’s still illegal to use state funds for syringes. Recently, GOP legislators attempted to require that programs secure public letters of support from law enforcement to operate. Meanwhile, overdose deaths increased by 45 percent between 2019 and 2020, forcing lawmakers to undo restrictions on naloxone. Buer also helps people who use drugs to form a political coalition. She calls it “movement building,” and her ambitions are to have space to facilitate organizing—such that when the city or state makes decisions that aren’t in the best interests of its most vulnerable, there’s a unified response.
“That’s my vision for the future,” Buer says.

Several times a month, Choice brings supplies to an unhoused encampment in downtown Knoxville. Greg Stafford, the outreach registered nurse, assists a client with supplies.

Hot Springs, North Carolina
Statewide overdose deaths 1999–2020: 29,081
Hot Springs is an iconic Appalachian Trail town—in fact, the trail weaves through the heart of downtown. In the back parking lot of the Dollar General, on the main drag, Ainsley Bryce, executive director of Holler Harm Reduction, is distributing life-saving assets.
Discretion is key. Most of these folks, after all, are struggling with addiction; they’d prefer to remain unobserved by law enforcement. Many struggle with shame. Bryce and her co-worker Alonza Lasher assure them: “You deserve an unused syringe, you deserve wound care, you deserve a friendly ear and love and support, regardless of anything.”

Friday is not a scheduled drop-in day, but Holler is not a stick-to-the-schedule type of operation. Alonza Lasher is waiting patiently for a woman, Denise, who has called ahead to ask about picking up syringes and a few other supplies for herself and sick or seven others. When she arrives, Denise, who is 44, reveals that ultimately she wants to get into treatment. She feels it could be successful, since she’s not a heavy user—just a gram or less a week of meth. “I feel like I’m not too far gone,” she says. “But I’m also not blind to the fact that I need to quit.”
Twenty-five miles northwest is the town of Newport, Tennessee, from where most of the people Holler is helping today have traveled. Choice Health Network used to operate a syringe exchange there, but their landlord kicked them out. Holler is now the closest option—North Carolina has relatively relaxed exchange laws—and for these folks it’s a godsend.
Business is brisk. Bryce dispenses her wares from the back of her truck. Folks linger a while to chat; many are her regulars and now friends. By the end of the day, she will have handed out more than 2,000 syringes.
Holler operates on a tight budget, one grant through AIDS United, another from an Asheville-based health trust. They haven’t applied for a federal grant. With a staff of three (Lasher and another worker are part time), they just don’t have the resources to slog through the application process, Bryce says. Meanwhile, they experienced a 4,000 percent increase in the number of people they serve, partly due to the exchange closure in Newport, but also to growing local awareness that their services are available.

Every Saturday, people from Newport, Tennessee, where a syringe exchange program was shut down, drive 25 miles to Hot Springs to receive supplies from Holler.

Nicole, a Holler client, shows Ainsley Bryce the lesions that have broken out on her legs. One of Holler’s services is care for wounds resulting from injection drug use.
In addition to scheduled drop-in days, they deliver supplies anywhere in the county, assisted by a few active users who extend Holler’s reach. Fifty-five-year-old Daisy is among them. She did a shot of cocaine at 18—“Scared the devil out of me”—and then nothing more till she was 42, in the course of a very bad year in which she got divorced and lost custody of her kids. She was suddenly alone. Then it was “cocaine, methamphetamine, pills,” whatever she could heat and put into a syringe.
Daisy overdosed on heroin three times in August 2012, was in recovery for five years, then started again after contracting lung cancer. She no longer injects, but she smokes meth. “I don’t get high anymore. It’s more like just maintaining the feeling of being okay.”

Daisy Dowling, 55, did a shot of cocaine at 18—”Scared the devil out of me”—and then nothing more until she was 42, in the course of a very bad year. Daisy overdosed on heroin three times in August 2012, stopped using again for five years, then started back after contracting lung cancer.
Daisy plays an important role in Holler’s network: She’s a link to people otherwise unlikely to find their services. She takes in young people who have no place to go. “If they need somewhere to lay down, they sleep at my house—and if they need food or a shower or whatever.” She brings home supplies and hopes that with her small interventions she might change the course of someone’s life. “It’s wrong for somebody who’s making bad decisions when they’re young to have to deal with it for a lifetime when you can give them what they need to be safe, and hopefully get out of it and move on,” she says.
Nicole is the last patient to come to the parking lot today. Having gathered her supplies, she talks to Bryce about her hopes of soon entering treatment. “Three months ago,” Nicole says, “this wasn’t in my heart. You couldn’t have made me stop if you wanted to. But it’s on my heart so strong…If I could just get my stuff together. Like I got reasons, but I can’t get it together.”
She’d recently gone six days without using, which is “a very long time for me.” Nicole isn’t sure where she’ll sleep tonight. Bryce urges her to be safe.
“It’s good to see you,” Bryce tells her. “Can I give you a hug before you go? Thanks for coming, dear.”
Nicole knows where to find her.
This story was produced in collaboration with the Economic Hardship Reporting Project and 100 Days in Appalachia.