Remigio RamirezWesaam Al-Badry/Contact Press Images
It was still dark outside when Veronica Perez arrived at Primex Farms, a nut packing facility in Kern County, California. Crickets murmured from the almond and pistachio groves stretching for miles in either direction. Inside the double doors, Perez, 42, usually stands next to other nut sorters alongside a conveyor belt and picks out the unseemly pistachios. But on June 25, at 4:30 a.m., Perez didn’t go in. Instead, for the next five hours, she and her colleagues formed a picket line. Some 30 employees joined on foot, with more circling and honking in their cars. They held homemade signs with the names of their infected coworkers. One sign in Spanish read, “The wise see danger and leave, but the foolish go on and suffer the consequences.” The employees chanted, “Somos esenciales!” We are essential.
In more than a decade of packing food in California, Perez had never joined a protest. But in recent months, things at Primex had become unbearable. In March, when employees concerned about the coronavirus requested to wear masks, Primex allegedly prohibited them from doing so, citing food safety concerns. When the company later allowed masks, instead of distributing them, it sold them for $8 apiece, according to several workers. (Primex denies ever selling masks.)
By early June, employees were falling ill. Those who stayed home sick reported not getting paid while they were out. Others kept coming to work, coughing and coughing. Meanwhile, Primex executives reportedly remained tight-lipped on any illness at their facility. “They said that they were going to let us know if anyone came down with it,” said maintenance worker Remigio Ramirez, “but they didn’t.”
When Ramirez told his boss in mid-June that he wasn’t feeling good, the supervisor “said we were short-staffed and needed more hands,” recalled Ramirez. It was probably just the flu, said the supervisor, urging Ramirez to take some medicine and come in.
A few days later, Ramirez, 54, was diagnosed with COVID-19. He stayed home, quarantining himself in his bedroom. “When I got up the next day, I didn’t see anyone—not my wife, not my daughters,” he said. “And I thought to myself, what’s happening? Did they leave me alone? But no, each one was in their room, sick.”

Veronica Perez
Wesaam Al-Badry/Contact Press Images
For many employees, the last straw came on June 23, when a local news channel reported that, according to Primex, 31 workers had tested positive for COVID-19. Employees watched the news in shock. Company leadership hadn’t told them about the cases, the first of which had been confirmed more than two weeks before. (Primex didn’t comment specifically on the lack of communication to employees, but said, “We began implementing [anti]-virus spreading steps long before the CDC guidelines were published. We are proud to say that we are one of the cleanest and most sanitized plants in the industry.”)
Primex was far from the only food production facility in the area where the coronavirus was spreading. Over the summer, the disease tore through the Central Valley, the vast, dry interior of California that produces a quarter of the nation’s food, including 40 percent of the country’s fruits and nuts. By mid-August, the Kern County fairgrounds had been transformed into a federal surge testing site, and more than 1 in 5 coronavirus tests were coming out positive. “The problem we’re seeing is not whether you’re going to get infected,” said Armando Elenes, secretary treasurer of the United Farm Workers (UFW) union. “It’s no longer a matter of if—it’s a matter of when.”
Primex is relatively small by California agribusiness standards. Roughly 400 employees work in its Kern County packing facility, processing about 6 percent of California’s pistachios each year. But despite the company’s size, its workers made a rare, risky decision with sweeping implications: While the pandemic has driven many vulnerable populations further into the shadows, Primex employees, many of whom are undocumented, took to the streets.
Perez knows this is not how the playbook is supposed to go. “Most workers prefer to keep quiet for fear of losing their jobs or for fear of retaliation,” she said. “I was amazed myself at the quick response we got from our coworkers. It may be that everyone is tired of always staying silent.”
Last month, I drove to the Central Valley to talk to agricultural workers about the effect of the rapidly proliferating virus on their lives. Nearly everyone I interviewed suspected that others they worked with had had the virus at one point. But no one wanted to bring it up with their coworkers or bosses: Just as pervasive as the virus is the secrecy around it.
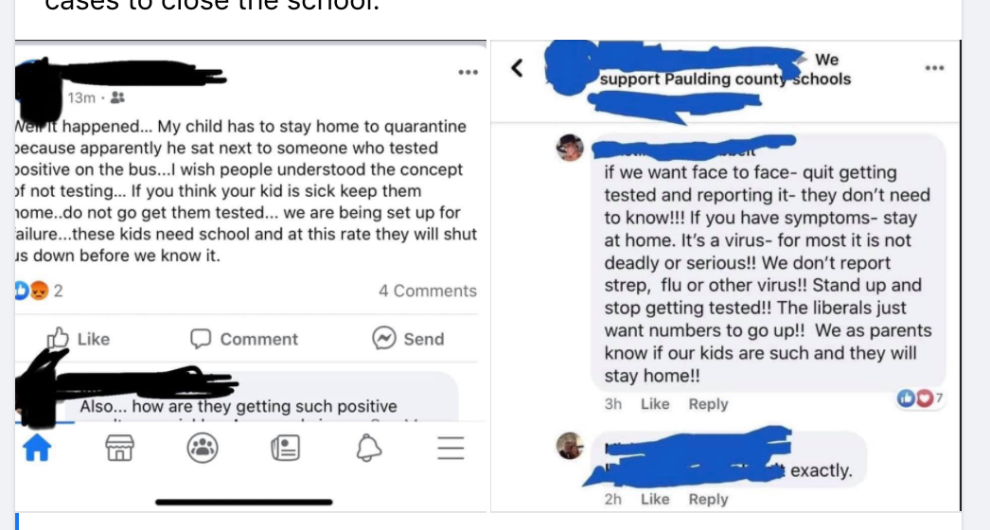
The mentality is, “if I feel good, even though I have the virus, I’m not going to tell you,” said one farmworker in Lost Hills. “The farm supervisors aren’t interested in if you have it or not. You might feel sick, but it’s fine—as long as you don’t die.”
An estimated half of the nation’s farmworkers are undocumented immigrants, according to the US Department of Agriculture. (Some estimate the rate to be significantly higher.) This open secret has long left farmworkers suspended in a contradiction: critical to feeding the country, yet deportable at the drop of a hat. With the pandemic, the dichotomy has only become more clear. Essential workers, including farmworkers, “have a special responsibility” to maintain normal work hours, according to President Trump’s guidance in March, yet undocumented workers don’t benefit from the federal coronavirus relief measures granted to citizens. (Those who are in the US on temporary work visas aren’t in a much better position: Some have been fired and lost their visas after getting the virus.)
Many agricultural workers now carry letters from their farms and packing plants identifying them as critical employees in case law enforcement picks them up. “I am a farm worker helping to protect our food supply during the Coronavirus pandemic,” read one such letter that a berry picker shared with me. “My job is considered essential so that we can produce food.”
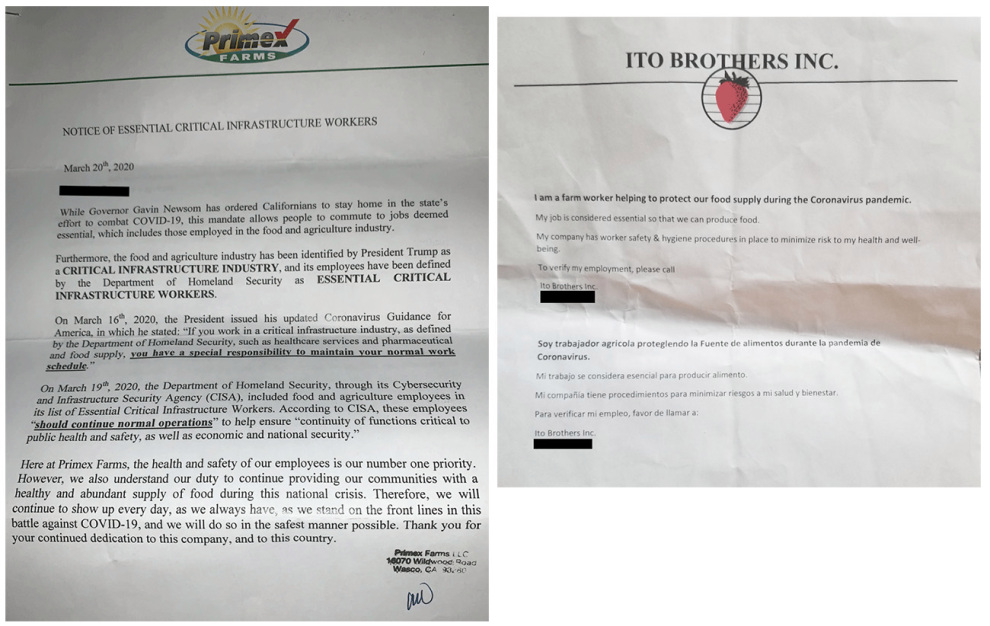
Many agricultural workers carry letters from their employers identifying them as essential during the pandemic.
Under federal coronavirus legislation and subsequent additions by California Gov. Gavin Newsom, many undocumented workers are eligible for two weeks of paid sick leave, deemed “COVID pay.” But in practice, enforcement is spotty. “If an employer is not paying them COVID pay, that sends a message to everybody else to not say anything,” said the UFW’s Elenes. And if an undocumented worker loses their job, they don’t get the unemployment stipend that the federal relief promises to other residents. “Most employees accept that they don’t have health insurance,” Elenes added. “But not having any income? That’s not something they can resolve.”
So begins a lethal feedback loop: The fear of lost wages and of immigration enforcement breeds silence, which in turn breeds transmission. “People are scared to say anything—or they take it like it’s a common cold, and they continue going to work,” said a 45-year-old who we’ll call Esperanza. Esperanza described a scene at her workplace, a plant nursery in Oxnard, similar to that at Primex: Over the summer, her coworkers started coming in sick, knowing they wouldn’t get paid if they stayed home. The nursery didn’t give out masks. But the worker response at the nursery was far less dramatic than that at Primex, and far more typical. Instead of protesting to demand better conditions or higher pay, workers simply went on working. Esperanza spoke to me over the phone in a quiet, cracking voice; just a couple weeks before, she had come down with the coronavirus.
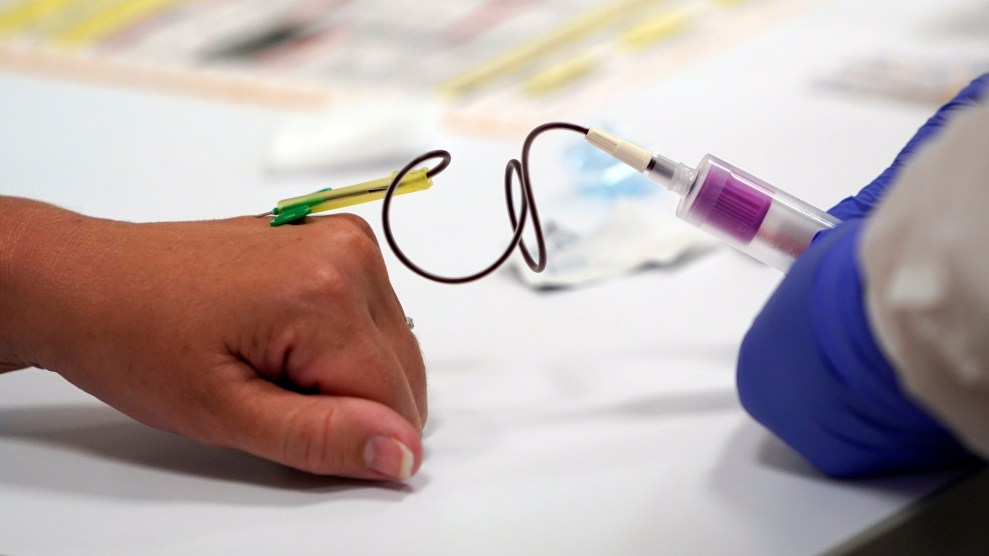
The fear also complicates COVID-19 testing efforts. Since mid-July, Kelly Gladden, a volunteer who spearheads a mobile coronavirus testing unit, has criss-crossed Kern County to test farmworkers. Since most other testing sites are far away from farms, and some workers don’t have transportation, the idea is to meet workers literally where they’re at. The operation was initially run out of a van, but the associations of a van with US Immigration and Customs Enforcement made Gladden change tacks. Now her team, a group from the Bakersfield-based Good Samaritan Hospital, sets up the testing tent in a field, between rows of grapes, or under the awning of a food processing or packing plant. Even still, the team encounters skeptics. Some growers don’t love the idea of using up work hours for testing, and some workers are afraid that their information will be shared, or that they won’t get paid if they test positive.
Fernando Perez, who works at a dairy outside of Bakersfield, explained that he purposely didn’t get a COVID-19 test when his coworkers, including his brother, came down with the virus. Perez, who is undocumented, didn’t want to risk the financial toll of testing positive—his brother wasn’t paid for his time at home. Plus, someone needed to operate the complex machinery to feed the cows. “If no one comes in, the animals don’t eat. If they don’t eat, they don’t produce,” he explained. “If we don’t go to work, 10,000 cows will die. Our work is very, very important.”
The shroud of silence adds to a host of environmental and situational factors that had already made agricultural workers perfect targets for the virus. Few farmworkers have regular access to health care. Many live with extended family members, with several generations under one roof, or in dormitories for temporary workers, where the virus proliferates. It’s common to carpool to job sites, some of which are greenhouses or packing houses with limited air circulation. Between the pollution from the pesticides, the oil fields, and the freeways, the Central Valley has atrocious air quality: Its largest cities, Bakersfield and Fresno, have the worst air particle pollution in the country, according to the American Lung Association. Rates of asthma, the fungal lung disease Valley Fever, and other respiratory ailments soar. It’s perhaps no surprise that, according to a recent Politico analysis, the nation’s key agricultural counties have disproportionately high coronavirus infection rates.
Making matters even worse, workers have had to contend with another hazard this month: A ring of fires around the Central Valley has turned the fields into a hot, soupy smog. “People look at us and don’t pay us much attention. We’re out in the rain, the heat, every other condition,” one worker told me. “They’re not taking into account that we need help.”
On Tuesday June 23, Perez, the Primex employee, sent a message to Elenes over Facebook. He was a near stranger, but she was desperate, reeling from the news of the COVID-19 cases at the company. At Elenes’ urging, Perez reached out to other concerned coworkers asking them to join a WhatsApp group, called Justicia en Primex Farms, and to invite their other colleagues. (Primex isn’t unionized, but the UFW organizes and advocates for agricultural workers in general, regardless of union status, said Elenes.) Within 24 hours, 100 people had joined. They gathered over Zoom the following evening, many using the video chatting platform for the first time, to plan a demonstration.

Farmworkers line up for Kern county’s mobile coronavirus testing unit
Kelly Gladden
When her coworkers showed up for the strike early Thursday morning, Perez was a jumble of emotions: thrilled that so many people had joined, terrified that they would face consequences. She carried a sign with a list of three demands: sick pay, job protection, and “respect.” Ramirez, the maintenance worker who’d tested positive the week before, showed support from the confines of his truck.
The effects of the demonstration appeared to be immediate. Later that day—more than two weeks after the first reported infection at Primex—the company closed for cleaning and announced it would contract with a mobile testing unit and implement other safety precautions, like installing plexiglass dividers at the sorting tables and more outdoor seating areas so employees on breaks could spread out.
When the company opened after a few days, workers gathered once again to protest. They alleged that Primex still wasn’t cleaning adequately or providing sick pay. This time, their numbers had grown to more than 60. But the demonstration lasted only a day. “We went back because we needed the work,” Perez said.
It was around that point that Elenes suggested employees start a coronavirus census, suspecting far more people than just the 31 that the company had reported were infected. Workers started coming forward in the chat, admitting they had tested positive. Since Primex is a 24-hour operation, the messages came in day and night. Elenes recalled waking up and finding message after message about positive tests among employees and their family members. One woman reported that not only was she infected, but 16 other family members were as well. The youngest was nine months old.
In the weeks after the protests, OSHA opened an investigation into the company; it remains open. But by that point, the virus was everywhere. Within three weeks, the employee census found that 97 of 400 employees were positive, along with more than 60 family members. The separate mobile testing unit provided by Primex would later find that 150 employees—more than a third of the plant’s workforce—had the virus.
In mid-July, a 57-year-old employee named Maria Hortencia Lopez was taken off life support and died of the coronavirus. Perez had known Lopez as a lively coworker on the assembly line who often brought in fruit to share and asked after Perez’s family. “I couldn’t believe that a person so full of life, such a happy and a good person, suddenly isn’t with you anymore,” she said.
Perez’s grief was undergirded by a quiet rage. She couldn’t shake the feeling that all of this could have been prevented. “That’s what hurts the most,” she said.
Just 25 minutes away from Primex sits Delano, where, in 1966, striking grape workers famously began the 340-mile march to protest the work conditions of farm laborers. The following decade marked a brief golden era for the UFW, with Cesar Chavez at the helm. At its peak, the union was 50,000 members strong, having secured in 1975 the California Agricultural Labor Relations Act, the nation’s only legislation allowing collective bargaining among farmworkers.
In the 1970s, the conditions at Primex “would have been an invitation to organize,” said Marshall Ganz, who directed organizing in the early years of the UFW and now lectures at the Harvard Kennedy School. “There’d be a grievance, and people would call out the union to come and help.”
Those days were short lived. Internal squabbling, fueled by Chavez’s increasing paranoia and refusal to decentralize power, seeded mistrust, and the union quickly found itself in a downward spiral. Fewer contracts were renegotiated, leaving those left behind to shoulder the costs. The successive Republican governor chipped away at state labor laws. Today, with just 7,500 members, the UFW is a shell of what it once was; it now represents less than one percent of farmworkers in California.
Recent months have brought blips of COVID-related organizing up and down the West Coast. Just a month before the Primex strike, hundreds of apple packers in Washington’s Yakima Valley walked off production lines to protest a lack of safety precautions and hazard pay. One worker inquired to Oregon Public Broadcasting, “Are their apples worth more than our lives?” The UFW is pushing for $2 per hour of hazard pay at poultry giant Foster Farms, which temporarily closed one of its California facilities this month after eight workers died of complications related to the coronavirus.
I asked Ganz: Could the pandemic lead to more organizing among farmworkers? “The whole question of where you find courage to take risks is always a question in organizing,” he said. “Where do you find courage to take risk? Grievances don’t generate courage. They generate anger or rage. They generate despair. So unless there’s some hope source, people don’t really engage. So then the question is, under these conditions, are there unusual or new sources of possibility? Hope isn’t about certainty at all—it’s just about possibility.”

Remigio Ramirez
Wesaam Al-Badry/Contact Press Images
But the reality is that hope is in short supply. In many ways, the pickers and packers of food in America find themselves facing the same challenges as the grape strikers of the 1960s: stagnant pay, perilous conditions, and backbreaking labor. The rate of farmworkers who are undocumented has shot up, from an estimated one in seven three decades ago to one in two today. Agribusiness companies increasingly rely on third party, hard-to-regulate staffing agencies to hire, transport, and house employees, notes University of California-Davis agricultural economist Philip Martin in his upcoming book, The Prosperity Paradox. This, combined with the eroded power of unions, makes agricultural workers today especially vulnerable. As Martin concludes, “Government enforcement of labor laws depends on complaints, and vulnerable workers rarely complain.”
At Primex, employees report that they are finally getting paid sick leave. Yet they told me that despite this small victory, the atmosphere at the plant has become increasingly oppressive.
On July 22, about a month after the first protest, dozens of workers lost their jobs when Primex canceled its contract with a temporary staffing agency. The company attributed the reduction to typical changes in seasonal production, but according to the UFW and Primex employees, the cuts included many of the most vocal workers. Primex promptly hired new workers to take the place of those who were terminated, prompting the UFW to file a complaint with the National Labor Relations Board. (The case is open; Primex declined to comment on the case but said of the UFW, “all they do is just play the blame game without any accountability.”)
In late July, a colleague of Perez’s tried to record a video inside the plant showing that that social distancing and mask wearing weren’t happening consistently, despite the company’s statements to the contrary. Primex disciplined the employee, according to another NLRB complaint, and the company required workers to sign a policy prohibiting video recording. Perez refused to sign. “That’s when [the production manager] pulled me into the office. He likes to scream a lot,” recalled Perez.

Workers arriving at the Primex facility early in the morning.
Wesaam Al-Badry
Later, Perez and Ramirez, the maintenance worker, were separately called into meetings with Primex’s manager of human resources and instructed to retract statements they made to the media over the course of the protests. Business was declining because of all the bad press, Perez and Ramirez were told—if the company went down, it would be because of employees like them. “They said, ‘This company should mean something to you,’” recalled Ramirez, who has worked at Primex for 13 years. As they spoke, he seethed, thinking about his sick wife and daughters.
Perez recalled the human resources manager “said her head was hurting from hearing me talk so much, and she didn’t want to hear from me anymore.” Despite the warnings, a lingering thought keeps Perez talking to reporters: “If it’s happening to this company, it could happen to a lot of other companies where there’s no one to talk.”
Some of the fallout from the demonstrations has been more subtle. Ramirez said that most of his remaining coworkers didn’t agree with his decision to strike, and they now say very little to him. Instead of regularly fielding requests for help, like usual, he now spends his work hours walking around, looking for broken things to fix. Another organizer was moved from operating a forklift inside to sweeping and painting outside in the sweltering heat. He’s considered quitting. “It’s hard to keep working there when the people who manage the plant don’t want you there,” he said.
At the end of July, Perez participated in a Facebook Live panel put together by Líderes Campesinas, an advocacy group for female farmworkers that she belongs to. She admitted to the group that things had been very difficult lately. Just that day, she’d been yelled at by the production manager for refusing to sign the policy against taking videos.
“I’m really short, and he’s tall,” explained Perez in Spanish. And then she began to weep. “It makes me want to cry because my coworkers—I’ve tried to be really strong in front of them, but I can’t anymore.” It seemed that when they spoke up, things got worse.
“We’re only asking for a safe place to work,” she exclaimed. “What do we have to do?”
This article has been updated. Camille Squires contributed to reporting this story.